Cancer:韩国多中心真实世界研究评估晚期或转移性非小细胞肺癌(NSCLC)免疫治疗的长期临床预后:KCSG LU20-11
2022-04-06 yd2015 MedSci原创
研究表明,晚期或转移性非小细胞肺癌(NSCLC)完成2年免疫治疗(ICI)或免疫治疗6个月后停药但没有进展患者可获得长期的生存预后。
近期,Cancer杂志上发表了一项来自韩国的多中心真实世界研究成果(KCSG LU20-11),主要是评估晚期或转移性非小细胞肺癌(NSCLC)完成2年免疫治疗(ICI)或免疫治疗6个月后停药但没有进展患者的长期生存预后成果。
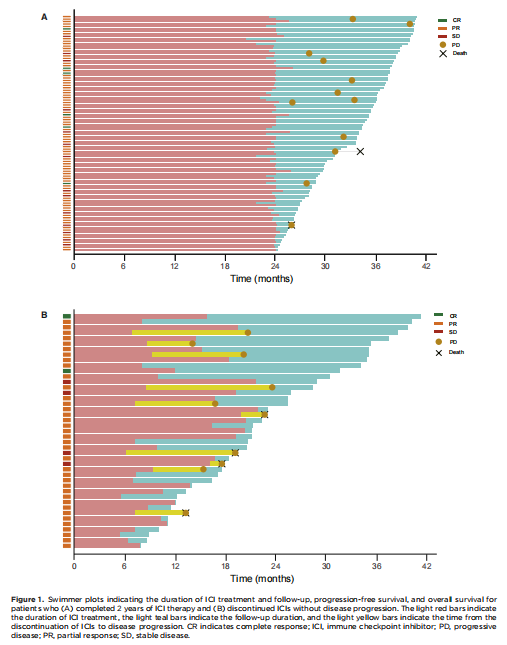
我们回顾性研究了来自韩国11个中心的139例晚期NSCLC患者(包括96例完成2年ICI治疗的患者和43例治疗超过6个月后停止ICI治疗且无疾病进展的患者)。ICI治疗始于2017年8月至2020年12月。
根据研究者评估,在完成2年ICI治疗的96名患者中,85.4%(82 / 96)的患者出现了缓解。最佳缓解分布如下:完全缓解(CR) 6例(6.3%),PR 76例(79.2%),SD 14例(14.6%)。
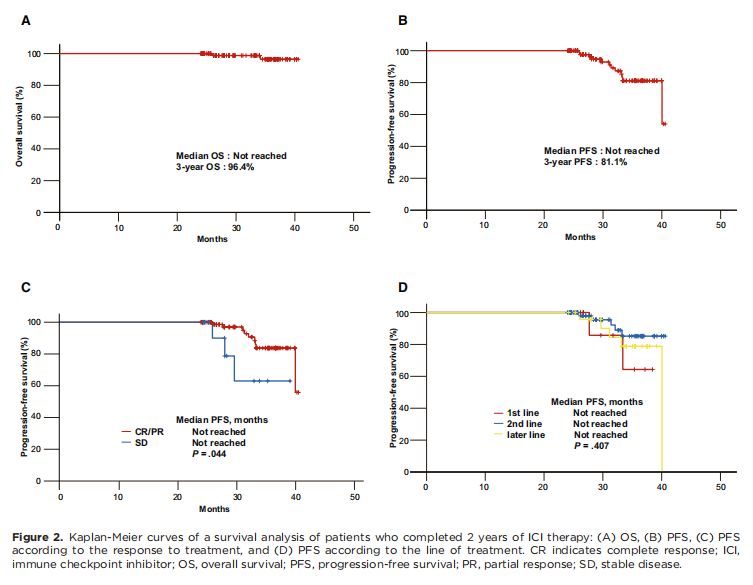
中位OS未达到,停用ICIs后12个月的估计OS率为96.4%。中位无进展生存期(PFS)未达到,ICIs停止后12个月的估计无进展生存期率为81.1%。获得ORR的患者的无进展生存期明显长于获得SD的患者(P =0.044)。从停药开始,获得CR和PR患者12个月的PFS和OS率分别为83.7%和97.4%,获得SD患者的分别为63.0%和90.0%。一线治疗、二线治疗或后线治疗的中位PFS均未达到(P = 0.407)。PFS在治疗的线数(P = .407)、ICI类型(P = .465)和PD-L1状态(P = .616)方面无显著差异。此外,OS在ORR (P = .076)、治疗的线数(P = .786)、ICI类型(P = .954)和PD-L1状态(P = .824)等方面也没有显著差异。
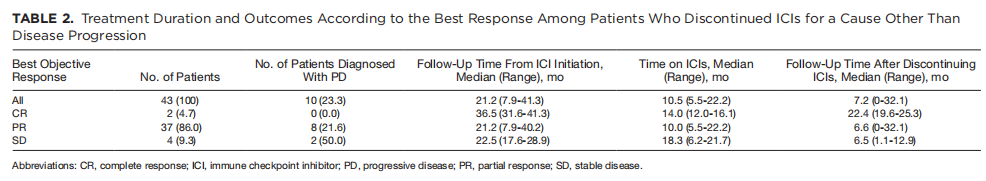
43例治疗超过6个月后停止ICI治疗且无疾病进展的患者中,中位治疗时间10.5个月,中位随访时间21.2个月。总体而言,90.7%的患者(39 / 43)获得缓解,最佳缓解分布:CR 2例(4.7%),PR 37例(86.0%),SD 4例(9.3%)。
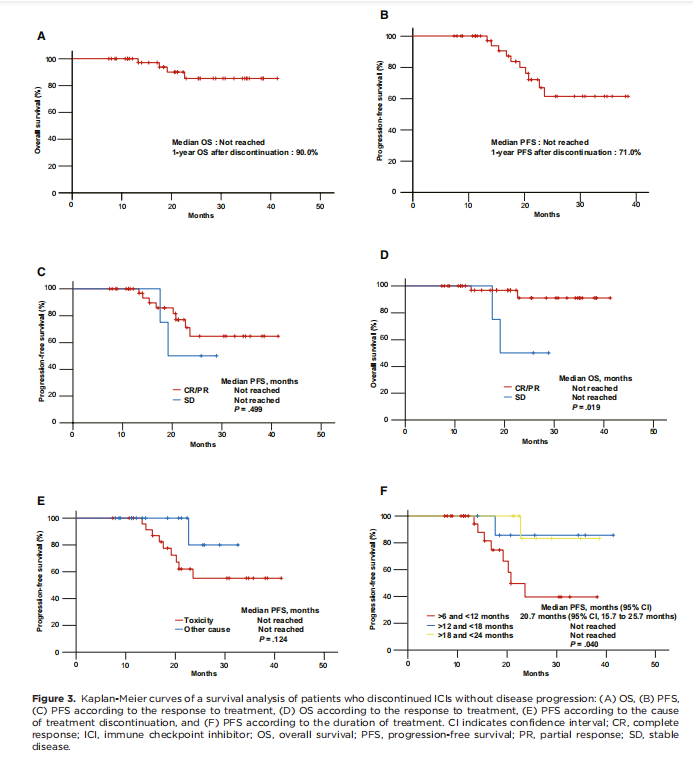
中位OS未达到,12个月的OS率为90.0%。中位无进展生存期未达到,12个月的PFS率为71.0%。获得CR和PR患者的中位PFS未达到,获得SD患者的中位PFS未达到(P = .499)。获得CR和PR患者的中位OS未达到,获得SD患者的中位OS未达到(P = .019)。因为AEs停药或因其他原因停药患者的中位PFS均未达到(P = .124)。应答持续时间6-12个月患者的中位PFS为20.7个月(95% CI: 15.7-25.7个月),12-18个月持续应答患者的中位PFS未达到,18-24个月持续应答患者的中位PFS未达到(P = .040)。
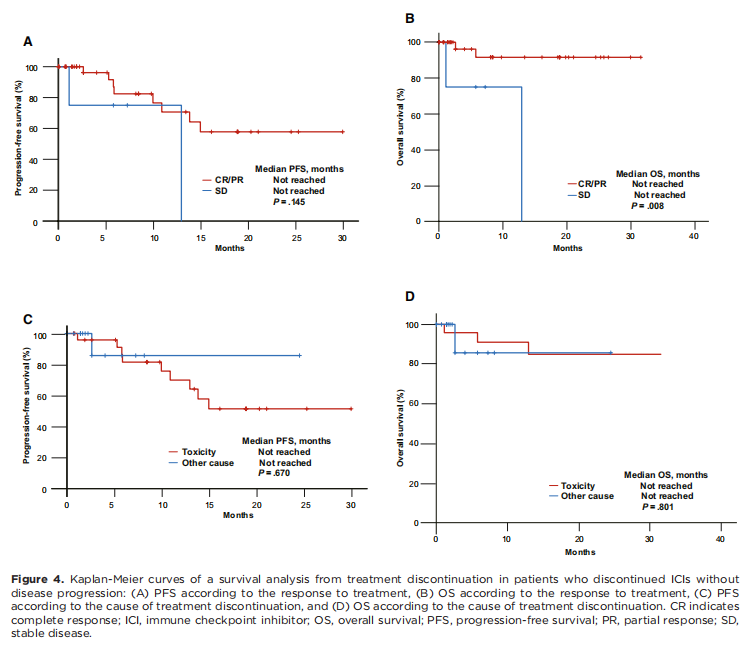
然而,中断ICIs后,获得CR和PR以及SD患者的中位PFS均未达到(P = .145);此外,获得CR和PR以及SD患者的中位OS均未达到(P = .008)。从ICIs的停止开始,因为毒性停药或其他原因停药患者的中位PFS均未达到(P = .670);此外,因为毒性停药或其他原因停药患者的中位OS均未达到(P = .801)。PFS在治疗反应(P = .499)、停药原因(P = .124)、ICI类型(P = .701)、治疗线数(P = .834)和PD-L1状态(P = .594)等方面无显著差异。此外,根据治疗线(P = .504)、ICI类型(P = .814)、PDL1状态(P = .145)和治疗时间(P = .963)等方面, OS也没有显著差异。
综上,研究表明,晚期或转移性非小细胞肺癌(NSCLC)完成2年免疫治疗(ICI)或免疫治疗6个月后停药但没有进展患者可获得长期的生存预后。
原始出处:
Kim H, Kim DW, Kim M, Lee Y, Ahn HK, Cho JH, Kim IH, Lee YG, Shin SH, Park SE, Jung J, Kang EJ, Ahn MJ. Long-term outcomes in patients with advanced and/or metastatic non-small cell lung cancer who completed 2 years of immune checkpoint inhibitors or achieved a durable response after discontinuation without disease progression: Multicenter, real-world data (KCSG LU20-11). Cancer. 2022 Feb 15;128(4):778-787. doi: 10.1002/cncr.33984. Epub 2021 Oct 27. PMID: 34705268.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#多中心#
114
#非小细胞#
86
学习了
97
#真实世界#
82
#韩国#
83
#转移性#
74
#转移性非小细胞肺癌#
96
#临床预后#
110
应该要区分亚型,不然意义不大
76