Nature:科学家阐明泌尿道感染复发的分子机制
2015-08-14 佚名 生物谷
当最佳抗生素消灭掉大多数引发泌尿道感染的细菌时,总会有一些细菌的“沉睡细胞”依然存活,而这些所谓的“持留菌”会在休眠中保持存活状态;近日一篇发表在国际杂志Nature上的研究论文中,来自杜克大学的研究人员通过研究发现,一种名为HipA的蛋白质或可扮演一种分子“睡魔”,其可以促使细菌细胞沉睡以便其可以躲避抗生素的杀灭作用,HipA的发现或可帮助开发抵御耐药性细菌感染的新型疗法。研究者Richard
当最佳抗生素消灭掉大多数引发泌尿道感染的细菌时,总会有一些细菌的“沉睡细胞”依然存活,而这些所谓的“持留菌”会在休眠中保持存活状态;近日一篇发表在国际杂志Nature上的研究论文中,来自杜克大学的研究人员通过研究发现,一种名为HipA的蛋白质或可扮演一种分子“睡魔”,其可以促使细菌细胞沉睡以便其可以躲避抗生素的杀灭作用,HipA的发现或可帮助开发抵御耐药性细菌感染的新型疗法。
研究者Richard G. Brennan博士表示,HipA的潜在突变体或许引发耐多药的泌尿道感染,本文研究或可帮助揭示突变如何增强HipA的潜力来帮助多种细菌避免被抗生素杀灭。如果我们可以寻找到一种新途径来阻断HipA的功能,那么或许就可以唤醒沉睡的细菌细胞,来利用抗生素对其有效杀灭。
当致病微生物设法生存或对抗生素攻击产生抗性时往往会引发细菌的多药耐受性,这种多药物耐受性并不能与多药抗药性混淆,在多药抗药性情况下,病原菌可以改变自身的遗传组成来对特殊药物产生耐受性;然而在多药耐受性情况下,微生物可以改变自身的行为,暂时关闭药物靶向作用的细胞功能,从而避免受到药物威胁。
研究者发现,HipA的突变形式HipA7产生的耐受性是一般耐药性的1000倍,研究者目前并不清楚HipA蛋白在人类疾病中所扮演的角色,为此研究者对来自泌尿道感染病人机体的多个大肠杆菌样本进行分析研究,并且对hipA基因进行了测序,结果发现,有将近24个样本都包含hipA7的高耐药突变,而且其对于引发患者出现多发性感染非常关键。
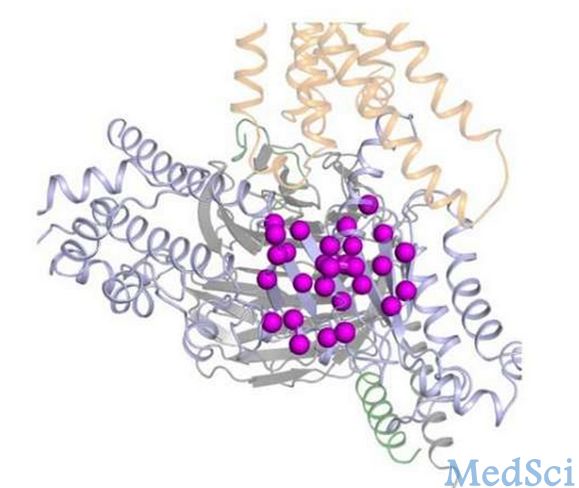
HipA可以扮演一类信号蛋白,“命令”其它蛋白质为其服务,为了观察hipA7的突变引发的效应,研究人员利用x射线晶体学技术对大量复合物进行了原子水平的三维结构成像,当HipA在信号途径中处于激活状态时,其就会作为一种单一分子或单体;当HipA同HipB结合时就会引发DNA沉默,当其配对或形成二聚物时,二聚体就会固定复合物,阻断HipA的活性位点。
如今研究人员阐明了为何某些细菌细胞对抗生素的作用没有任何反应,研究者后期将会开发新型疗法来靶向作用这种多药耐受性的特殊分子机制,而研究者也将会寻找新型分子来促进HipA失活以便阻断其帮助细菌细胞休眠,进而有效治疗泌尿道感染的患者。
原文链接:
Maria A. Schumacher, Pooja Balani.et al.HipBA–promoter structures reveal the basis of heritable multidrug tolerance.Nature.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#尿道#
88
这篇文章有一定深度
231
是一篇不错的文章
179
很值得学习
165
#Nat#
73
#尿道感染#
97
分子方向的研究,热门
166
怪不得这么不好治疗呢
196
分子机制并不代表临床的机制
70
不置可否
91