联动成像技术 (linked color imaging,LCI) 是一种新型图像增强内镜技术,目前已在临床上逐步应用。多项研究证实,LCI 可通过增加内镜下病变黏膜和正常黏膜的对比度来提高对消化道黏膜病变的诊断准确率。
LCI 技术自 2015 年在中国上市以来,已广泛应用于消化道黏膜疾病的筛查。LCI 将特定短波长窄 带光与白光相结合照射在黏膜表面,在保证视野光 亮度的同时凸显黏膜表层血管、表层构造的信息。

图:LCI 基本颜色特性 ( 红线虚框范围 )
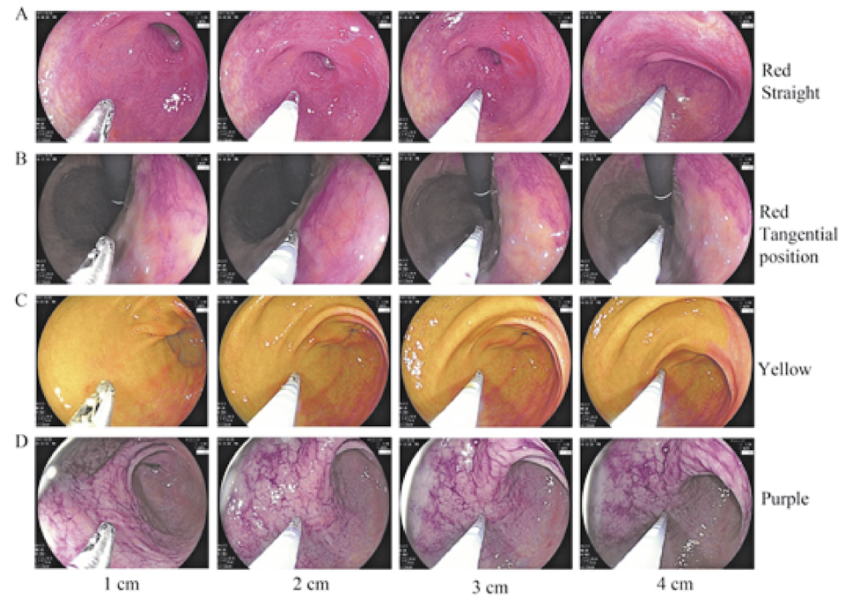
图:LCI 基本颜色随距离变化情况
同时,LCI 模式对色彩进行再度配置,加入红色强调信号后,使得黏膜颜色对比度增强,能够更好地识别黏膜颜色的微小色差,进一步增加了消化道病变的检出率。
LCI 模式可以和白光模式结合应用,筛查胃内病变
白光内镜可发现绝大部分胃黏膜病变, 但是对于一些微小病变则容易漏诊。LCI 在不影响 其图像亮度的前提下仍可保持良好的光学染色,因此可用于对胃黏膜的整体远景观察。
在内镜检查时,LCI 可更加快速和准确地发现可疑病灶,有利 于缩短操作时间。目前,有意见推荐先行 LCI 和 白光结合观察,发现病灶可疑区域,后再行放大内镜 检查观察病灶细节。
LCI 有助于诊断幽门螺杆菌感染
正常胃黏膜在白光内镜下可见排列规则的集合细静脉, 而 LCI 模式强调集合细静脉色彩而使其更容易被观 察,从而为诊断幽门螺杆菌感染提供重要信息。幽门螺杆菌感染后胃黏膜可出现胃固有腺萎 缩、肠上皮化生等慢性改变。应用白光内镜有时较难 对萎缩边界、弥漫性发红和平坦型肠上皮化生等进 行诊断。LCI 模式更容易观察到萎缩边界。鉴于 LCI 在观察黏膜形态和颜色细微改变的独特优势,其 对判断幽门螺杆菌临床感染有重要的应用价值。
LCI 可用于诊断胃黏膜肠上皮化生
尽管利用普通白光内镜可观察到肠上皮化生,但是 在普通白光很难快速判断肠上皮化生的边界。在 LCI 模式下,肠上皮化生呈淡紫色,又称为薰衣草紫 (lavender purple)、“氤氲紫”(purple in mist,PIM),与 红色调非肠上皮化生黏膜色彩明显不同,因而 LCI 模式可应用于肠上皮化生的诊断。
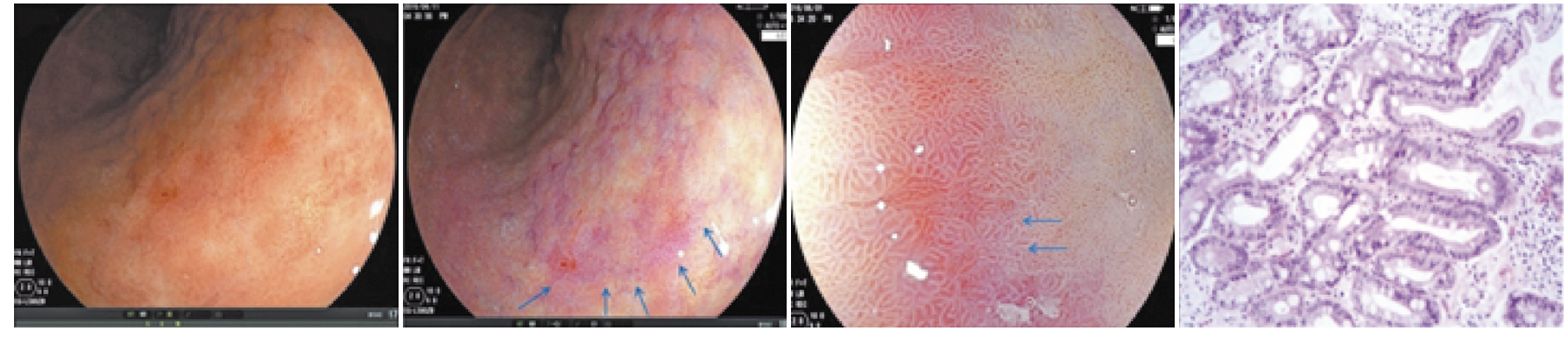
肠上皮化生的 LCI 表现
白光内镜下肠上皮化生表现为黏膜略发白和粗糙,可呈颗粒状或凹凸不平,而 LCI 通过对病变形态学的观察和 颜色调的识别来实现双重诊断。淡紫色诊断肠上皮 化生的效率较高,其准确率可达 80% 以上,但需要 与黏膜下血管呈现的紫色相鉴别,主要可通过大 体形态进行鉴别。
LCI 可用于筛查早期胃癌
胃癌常发生于慢性炎症的背景下,因此早期胃癌病灶可被周围 背景黏膜所掩盖,即使使用高分辨率内镜也很难诊 断。LCI 强调不同黏膜表面的色彩,观察肠上皮化 生黏膜呈淡紫色调,肿瘤病灶呈红色或白色,这样更易识别早期病变。
LCI 在兼顾观察病 灶形态学改变的同时,重点强调胃黏膜病变的颜色 改变。初步建立了 LCI 模式下胃“CVS”内镜诊 断流程,对于黏膜呈红色并有凹陷型特征病灶提出 了相关诊断标准,即 LCI 下观察到红黄混合或混杂, 提示早期胃癌 ;如病灶周围观察到淡紫色背景,则 提示分化型早期胃癌,如未观察到淡紫色背景,则提示未分化型可能性大。需在颜色诊断的基础 上,进一步结合放大内镜对微血管和微结构的诊断 标准,进行早期胃癌诊断。
LCI 可以用于无蒂锯齿状腺瘤和 ( 或 ) 息肉 (SSA/P) 的筛查
结直肠息肉和 SSA/P 属于 结直肠癌前病变,利用结肠镜筛查并切除病变,能够 有效降低结直肠癌发病率。有研究利用静态图像检查和前瞻性的随机对照试验发现 LCI 较白光、BLI、 BLI-bright 对 SSA/P 的检出率最为敏感,同时能够 提高专家及非专家内镜医师的 SSA/P 检出率。

图:白光和 LCI 模式下发现息肉对比
针对溃疡性结肠炎 (UC) 内镜下评分,建立 LCI 分类体系,用于评估 UC 结肠黏膜愈合程度及预测复发率
内镜下评估 UC 结肠黏膜愈合程度是判断 UC 活动程度、治疗目标、预后和临床治疗 终点的重要依据。目前 UC 黏膜愈合判断主要通过 传统白光内镜,内镜下黏膜愈合的质量可作为评估 UC 复发的主要预测因素。
LCI 模式下可以参照 NICE 分类系统预测结肠息肉组织病理学
目前对于结肠息肉内镜 下分型,NICE 分类系统被广泛运用于临床实践中。 有研究回顾性分析,在 LCI 模式下,可以参照 NICE 分型对 43 例患者结肠息肉的病理类型进行预测, 结果发现,肿瘤病变预测的敏感度、特异度、阳性预 测值和阴性预测值分别为 96.5%、83.8%、90.2% 和 93.9%。
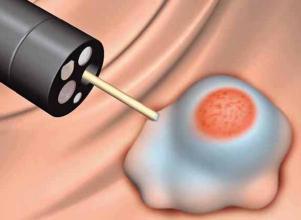
LCI 模式下进行结肠息肉切除前的黏膜下局部注射,避免误伤血管
黏膜下局部注射 是内镜下结肠息肉高频电切术、内镜下黏膜切除术 (EMR) 的一个关键步骤,也是后续手术的基础。适 当的黏膜下注射可提高内镜下治疗的有效性、安全性。然而,在黏膜下注射过程中,若损伤白光不可见 的浅表血管有时会引起血肿形成,从而增加后续切 除的困难。LCI 与白光、NBI 等技术相比,能更加清 晰地显示黏膜表层的血管,有助于精确定位注射的 安全位置,从而避免损伤病变周围的血管,防止不必 要的出血和血肿形成。
LCI 模式确定大肠侧向发育型腺瘤 (LST)病变边界
LST 具有较高的癌变潜能,由于其沿结肠黏膜侧向性发展而非垂直生长, 因此即使发生癌变,其发生血管侵袭及淋巴结转移 概率也较低,且大部分为黏膜内癌,向深部浸润者较 少。由于大部分 LST 直径大于 2 cm,内镜下准确判断边界对保证病变完整切除意义重大。另外,不推荐在 LCI 模式下进行结直肠黏膜病变黏 膜下剥离术,推荐应用 LCI 模式观察术后创面,预防出血及止血。
原始出处
1,谢聪颖 , 刘岩 . 联动成像内镜的原理及临床应用现状 [J]. 中华 消化内镜杂志 , 2017, 34(8): 600-602.
2,Osawa H, Miura Y, Takezawa T, et al. Linked color imaging and blue laser imaging for upper gastrointestinal screening[ J]. Clin Endosc, 2018, 51(6): 513-526.
3,国家消化道早癌防治中心联盟.消化内镜联动成像技术临床应用建议.中国实用内科杂志.2019 年 3 月.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#胃肠病#
95
学习到了
110
#内镜#
0
谢谢老师
111
学到了很多东西,谢谢老师的指导
97
装备再好,也躲不过认认真真
94