Cancers:保乳治疗较全乳切除术改善I-IIA期乳腺癌患者的预后
2021-08-12 越多015 MedSci原创
该研究表明,与单纯全乳房切除术相比,BCT显示有更好的DFS,强调了辅助治疗(包括术后放疗)在早期乳腺癌患者的重要作用。
一些随机对照试验的长期随访数据显示,乳房切除术与保留乳房治疗(BCT)(包括肿瘤切除术或四分之一乳房切除术,随之术后放疗)在无病生存(DFS)、远处无病生存和总生存期(OS)没有没有明显差异。因此,近期有团队比较了1360例早期乳腺癌(I-IIA期)患者根据局部治疗类型的生存结果。相关结果发表在Cancers杂志上。

该研究纳入2001至2013年期间诊断的1360例I-IIA(T1–2N0 or T0–1N1)乳腺癌患者,其中接受保乳治疗(BCT)1021例 (75.1%) 和单纯全乳房切除术339例(24.9%)。大部分乳腺肿瘤大小≤2cm (n = 1100, 81.5%),ER或PR阳性(n = 1241,92.3%)。与BCT组相比,全乳房切除术组接受紫杉烷类化疗的频率更高(32.8% vs . 24.7%;p<0.0005)。与仅接受全乳房切除术的患者相比,接受BCT的患者更常接受芳香化酶抑制剂辅助内分泌治疗(n = 141;40.3% vs n = 437;46.9%),接受他莫昔芬辅助治疗的可能性更低(43.4% vs 41.5%)。观察到的差异有统计学意义(p <0.0005)。
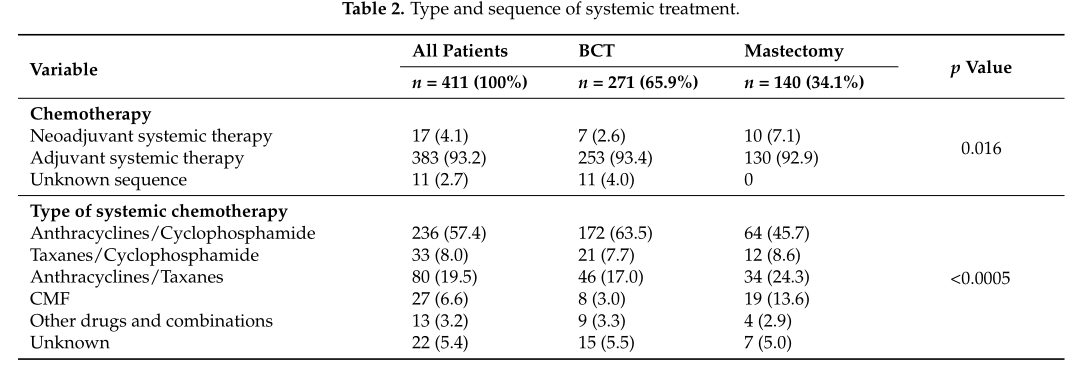
术后治疗对比
中位随访DFS和OS分别为6.9年(范围:0.3-15.9)和7.5年(范围:0.2-25.9)。分别有15例(1.1%), 14例 (1.0%) 和48例 (3.5%) 患者分别经历局部(LR),区域(RR)和远处转移。BCT组的5年和10年的LR率分别为1.0% 和 3.0%;全乳切除术的5年和10年的LR率分别为4.0% 和 4.0%。
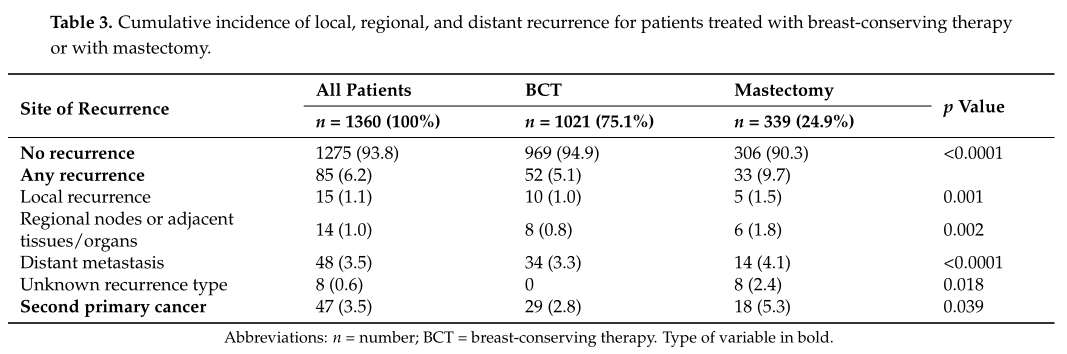
进展模式
BCT组的5年和10年的DFS率分别为97% 和 96%, 而单纯全乳切除术91%和90% (log-rank; p < 0.001)。在单因素分析中,以下因素与DFS降低有关:未接受BCT、年龄>70岁,肿瘤大小≥2cm, IIA期,肿瘤分级≥2级,不进行内分泌辅助治疗。多因素Cox分析显示,局部治疗类型和肿瘤分级仍持续具有统计学意义。
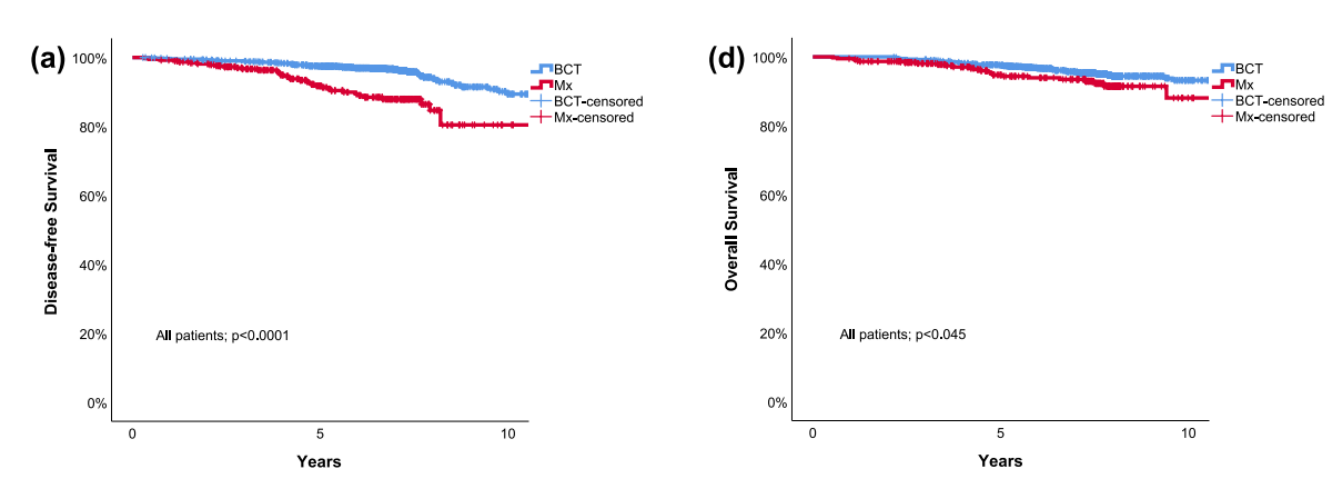
DFS和OS
BCT组的5年和10年的OS率分别为97% 和93%, 而单纯全乳切除术95%和89% (log-rank; p=0.045)。单因素分析发现全乳房切除术作为唯一的局部治疗与OS较差相关,但多因素Cox回归分析并没有统计学差异。全乳切除术与较差DFS相关 (HR=2.839, 95% CI 1.760–4.579, p < 0.0001),但是与OS无明显相关 (HR 1.455, 95% CI 0.844–2.511, p = 0.177)。
目前也有多项研究发现保乳治疗(BCT)较全乳房切除术改善患者的预后。
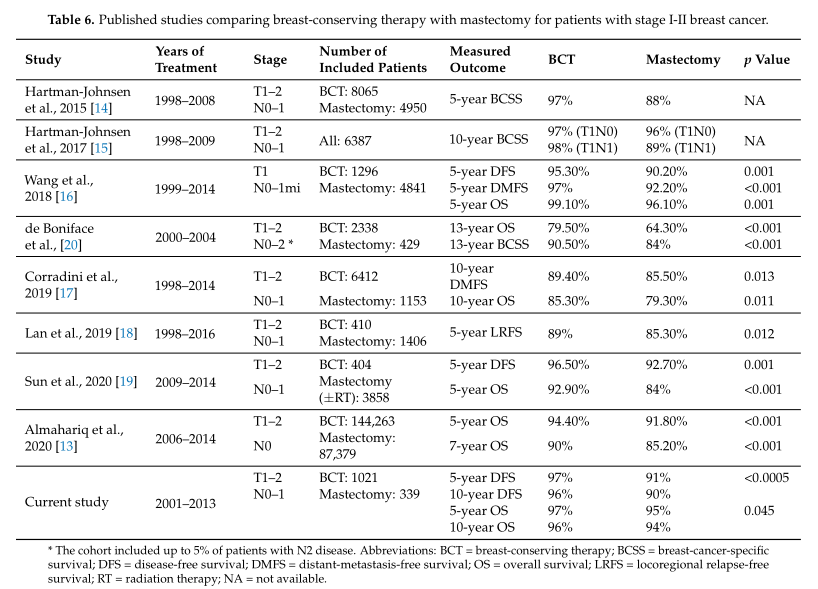
已发表相关研究
综上,该研究表明,与单纯全乳房切除术相比,BCT显示有更好的DFS,强调了辅助治疗(包括术后放疗)在早期乳腺癌患者的重要作用。
原始出处:
Ratosa, I.; Plavc, G.; Pislar, N.; et al. Improved Survival after Breast-Conserving Therapy Compared with Mastectomy in Stage I-IIA Breast Cancer. Cancers 2021, 13, 4044. https://doi.org/10.3390/ cancers13164044.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ERS#
24
#切除术#
33
#全乳切除#
34
#乳腺癌患者#
33
学习了
43