Nat Commun:老年痴呆治疗新方法
2015-08-21 佚名 生物谷
阿尔茨海默氏症会影响中枢神经系统,淀粉样蛋白块的形成进而导致慢性炎症,最终导致神经损伤。针对这种病症的很多免疫抑制类药物都失败了,还没有很好的方法能够治疗这种疾病。之前的研究已经发现,当将免疫细胞朝向中枢神经系统引导时,这些症状会减轻,在动物模型中这个现象已经得到了验证。也就是说自身免疫系统能够被用来缓解阿尔茨海默氏症带来的症状。但是具体如何引导免疫系统,如何利用自身细胞来消化这些淀粉
阿尔茨海默氏症会影响中枢神经系统,淀粉样蛋白块的形成进而导致慢性炎症,最终导致神经损伤。针对这种病症的很多免疫抑制类药物都失败了,还没有很好的方法能够治疗这种疾病。之前的研究已经发现,当将免疫细胞朝向中枢神经系统引导时,这些症状会减轻,在动物模型中这个现象已经得到了验证。也就是说自身免疫系统能够被用来缓解阿尔茨海默氏症带来的症状。但是具体如何引导免疫系统,如何利用自身细胞来消化这些淀粉样蛋白颗粒,一直都是一个难题。
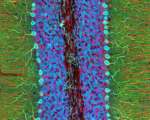
以色列魏茨曼科学研究所的科学家们在最近一期Nature Communications上发表的一项研究,阐述了一种新方法可能可以治疗阿尔茨海默氏症。他们的这项研究显示,通过以在调控身体免疫系统中起重要作用的特定免疫细胞(调控性T-细胞)为治疗目标,阿尔茨海默氏症的关键症状在小鼠身上可以得到缓解。
在这篇研究论文中,Michal Schwartz及同事发现,阻断特定Foxp3+调控的T-细胞(被称为Foxp3+ Tregs)的活性,可以使更多免疫细胞朝着小鼠的脑部区域移动。通过使用Foxp3+调控的T-细胞缺陷的小鼠模型,或者使用药物抑制Foxp3+调控的T-细胞的活性,都发现了,在小鼠中,淀粉样蛋白颗粒逐渐消失。同时,研究人员还观察到,小鼠的炎症反应也减少了,实验中小鼠在认知试验的测试中表现相对于没有抑制Foxp3+调控的T-细胞的情况有了好转。他们还发现,短暂性Foxp3+调控的T-细胞缺陷的小鼠中,免疫细胞运输到中枢神经系统的选择性通路受到了影响,这可能进一步解释了免疫细胞朝着中枢神经系统转移的现象。
以色列科学家的这项研究显示了,通过调控性T-细胞活性,能够影响免疫细胞在不同组织器官的转移,进而可能会大脑的神经系统相关疾病的进程。此外,这个研究还证明了,Foxp3+调控的T-细胞是未来治疗阿尔茨海默氏症的可能药物目标,通过抑制这种细胞的活性可能会给阿尔兹海默症的药物研发提供新的希望。
原文出处:
Kuti Baruch,Neta Rosenzweig.et al.Breaking immune tolerance by targeting Foxp3+regulatory T cells mitigates Alzheimer’s disease pathology.Nat Commun.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#新方法#
41
#Nat#
42
#COMMUN#
0
#治疗新方法#
43
我喜欢
119