Nature Neurosci:睡眠差居然与老年痴呆相关
2015-06-05 佚名 生物谷
来自加州大学伯克利分校的研究人员们发现老年痴呆症的beta-淀粉样蛋白沉淀,与睡眠差(尤其是非快速动眼期睡眠的中断)及大脑的长时期记忆力减退有关。这项研究揭示了老年痴呆症引起记忆力下降的一种可能的方式,即影响睡眠。相关研究结果于近日在线发表在Nature Neuroscience杂志上。 在此项研究中,研究人员们利用了正电子发射断层扫描(PET)来测量大脑中beta-淀粉样蛋白的沉积量;用功
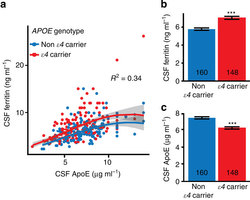
来自加州大学伯克利分校的研究人员们发现老年痴呆症的beta-淀粉样蛋白沉淀,与睡眠差(尤其是非快速动眼期睡眠的中断)及大脑的长时期记忆力减退有关。这项研究揭示了老年痴呆症引起记忆力下降的一种可能的方式,即影响睡眠。相关研究结果于近日在线发表在Nature Neuroscience杂志上。
在此项研究中,研究人员们利用了正电子发射断层扫描(PET)来测量大脑中beta-淀粉样蛋白的沉积量;用功能性磁共振成像(fMRI)来检测大脑在记忆活动中的活性;用脑电图(EEG)来记录大脑在睡眠时的脑电波;最后,他们利用统计模型来分析所有的数据。
研究人员招募了26名年龄在65到81之间的老年人,他们没有痴呆症,神经退行性病变,睡眠或是精神障碍。首先,这些老年人接受了正电子发射断层扫描(PET),来测量他们大脑中beta-淀粉样蛋白的量。接着,他们被要求记住120个词组,并且检验他们最终记住了多少个。在接下来的8小时睡眠中,脑电图记录了他们的脑电波。第二天早上,这些老年人被要求回想昨天记住的词组,同时他们的大脑接受了功能性磁共振成像的检测,此时,可以检测到大脑海马区域的活性,短暂的记忆被储存在这里,之后这些记忆被传送到前额叶皮层。结果显示,参与者中内侧额叶皮层的beta-淀粉样蛋白最高者,睡眠质量最差,而且,在第二天的词组记忆测试中,参与者忘记了一半以上的前一天所记住的词组。
此项研究提示,大脑中越多的beta-淀粉样蛋白,会导致睡眠质量越差,结果,记忆力也越差。而且,越差的睡眠,也会反过来导致大脑清除这些有害的蛋白的能力越差,这是一种恶性循环。然而,低质量的睡眠和有害的蛋白,哪一个因素是此恶性循坏的起始点,现在仍不清楚。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












这篇文章有一定深度
151
是一篇不错的文章
92
#Nat#
59
看来我有有AD的危险
151
以后睡好点啊
111
?
190
#ROS#
80