J Hepatology:酮康唑通过下调肝细胞癌中的环氧合酶-2来加剧线粒体自噬以诱导细胞凋亡
2018-12-17 MedSci MedSci原创
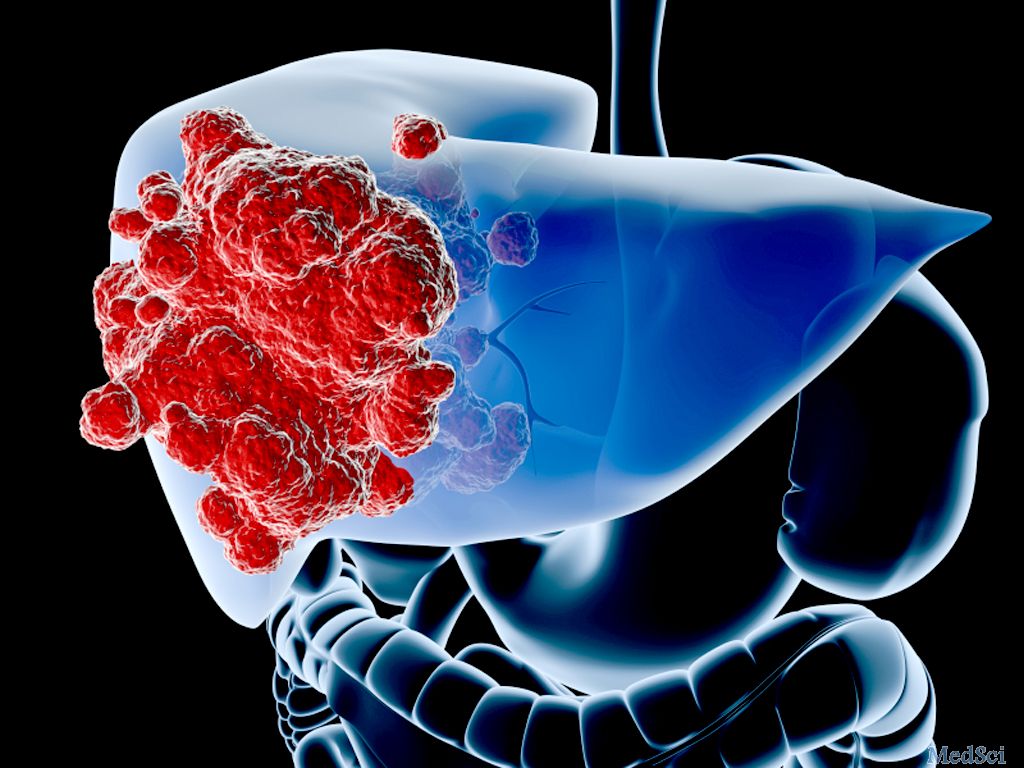
肝细胞癌(HCC)是世界范围内的比较常见的癌症,而酮康唑是一种传统的抗真菌剂,是否可以作为癌症治疗的药物目前引起相当大的关注,其作用机制仍未明确。因此本项研究旨在评估酮康唑对HCC的作用并研究其潜在机制。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肝细胞#
63
#细胞癌#
47
#细胞凋亡#
51
#EPA#
53