Movement disorders: 孤立快速眼动睡眠障碍,铁代谢障碍,可预示其表型变化
2022-02-15 Freeman MedSci原创
血清CDT的降低与突触蛋白病的黑质变性有关
近年来,帕金森病(PD)的诊断方法已经从经典的运动障碍观点发展到了一种具有长潜伏期的系统性疾病,此时亚临床的突触蛋白病表现为非运动症状,可以比主要运动症状的出现早几十年。孤立的快速眼动睡眠行为障碍RBD(iRBD)是一种以生理性快速眼动睡眠骨骼肌失张力和梦境颁布行为丧失为特征的寄生性失眠,是突触核蛋白病最特殊的前驱症状,这些患者中几乎有一半会转化为PD。在最近的一项多中心研究中,黑质多巴胺能的丧失被证明是早期症状转化的最有力预测因素。
 然而,多巴胺转运体单光子发射计算机断层扫描(DaT-SPECT)是一种昂贵的检查,与辐射暴露有关,这使其无法用于密切的纵向监测。找到更方便的早期转化的血源性标志物将允许对即将转化的患者进行更灵活的分层。牵涉到PD病理生理学的因素之一是黑质中的铁积累,据称这加速了自由基的产生,并可能导致黑质系统的功能损害。有趣的是,一项荟萃分析表明,与对照组相比,PD患者脑脊液(CSF)中的铁含量可能增加,而血清中的铁含量可能减少。转铁蛋白是主要的铁运输蛋白,它也能以其高含量将铁从组织中运走。许多针对不同人群的研究表明,转铁蛋白及其受体基因多态性可以改变PD的风险。因此,了解转铁蛋白的微异质性可以更好地了解PD的发病机制。
然而,多巴胺转运体单光子发射计算机断层扫描(DaT-SPECT)是一种昂贵的检查,与辐射暴露有关,这使其无法用于密切的纵向监测。找到更方便的早期转化的血源性标志物将允许对即将转化的患者进行更灵活的分层。牵涉到PD病理生理学的因素之一是黑质中的铁积累,据称这加速了自由基的产生,并可能导致黑质系统的功能损害。有趣的是,一项荟萃分析表明,与对照组相比,PD患者脑脊液(CSF)中的铁含量可能增加,而血清中的铁含量可能减少。转铁蛋白是主要的铁运输蛋白,它也能以其高含量将铁从组织中运走。许多针对不同人群的研究表明,转铁蛋白及其受体基因多态性可以改变PD的风险。因此,了解转铁蛋白的微异质性可以更好地了解PD的发病机制。
转铁蛋白的异质性是由以下因素造成的:(1)遗传变异;(2)附着的铁离子数量;以及(3)由不同程度的分支、末端糖残基和西亚利基化水平所决定的碳水化合物分子的差异。根据唾液基化的差异,九个含有零到九个唾液基酸残基的转铁蛋白同型被认可。含有零、一个或两个唾液酸链的转铁蛋白被统称为碳水化合物缺乏的转铁蛋白(CDT)。CDT被发现在酒精中毒患者的脑脊液和血清中升高,并已成为酒精使用障碍的一个重要标志物。
蛋白质唾液酸化的失调已被牵涉到神经退行性疾病中。在PD中,单唾液酸化的外周IgG的比例减少。在PD中还描述了不同形式的转铁蛋白的硫酸盐化。当比较CSF水平时,与未经治疗的PD患者和对照组相比,多巴胺能治疗的PD患者的水杨酸化程度明显较低,以sialylated形式为主,tetrasialylated形式减少。在血清中,与对照组相比,PD患者的转铁蛋白异构体的比例向更高的硅醛化形式转移。然而,目前还不知道转铁蛋白水杨酸化的改变是前驱滑膜病的早期标志还是完全发展的障碍的后期标志。
藉此,布拉格的Ranjani Ganapathy S等人,探究了CDT是否可以成为前驱性突触神经病的生物标志物,检查它与其他临床和影像参数的关系,并检查它是否有可能成为iRBD中表型转换的预测因素。
他们纳入了60名治疗无效的PD患者;72名经多导睡眠图确认的孤立性快速眼动睡眠行为障碍(iRBD)患者,即前驱性突触病患者;以及46名年龄≥45岁、每月饮酒量≤60标准杯的健康志愿者。使用高效液相色谱法评估血清中低水杨酸化、碳水化合物缺乏的转铁蛋白( serum low-sialylated, carbohydrate-deficient transferrin (CDT)异构体的比例,并根据酒精摄入量调整该值(CDT-adj )。进行了多巴胺转运体单光子发射计算机断层扫描(DaT-SPECT)成像。在iRBD中,使用Cox回归对年龄和性别进行了调整,评估了DaT-SPECT和CDTadj的酚醛转化风险。
他们发现:与对照组(1.2 [1.1-1.6]%)相比,PD的中位CDTadj更低(1.1 [四分位数范围:1.0-1.3]%)(P = 0.001)。
在iRBD中,DaT-SPECT异常(1.1 [0.9-1.3]%)的受试者的CDTadj中值低于正常(1.3 [1.2-1.6]%)(P = 0.005)。
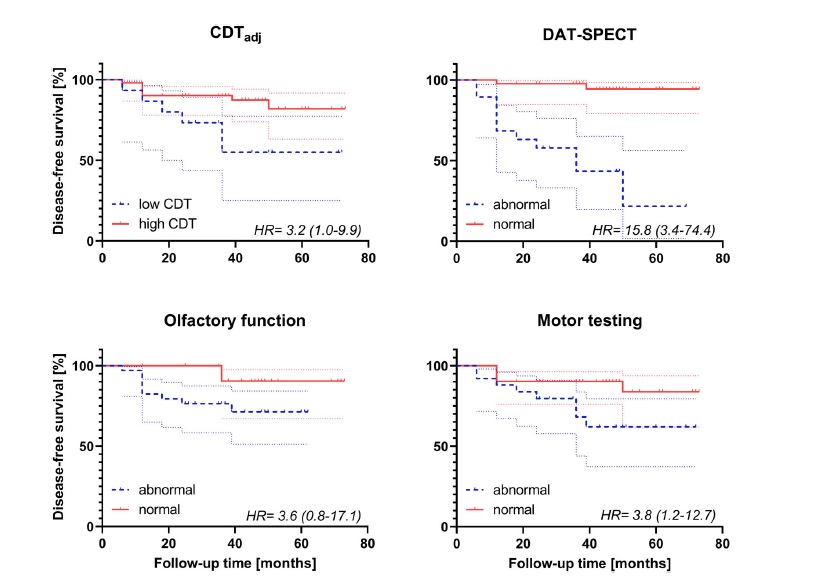
经过中位数44个月的随访,20%的iRBD患者进展为明显的疾病。尽管iRBD转换者和非转换者在CDT-adj水平上没有明显差异(P = 0.189),但低CDT-adj增加了表象转换的风险,危险比为3.2(P = 0.045),但没有细化与异常DaT-SPECT产生危险比15.8(P < 0.001)的表象转换风险。
该研究的重要意义在于发现了:血清CDT-adj的降低与突触蛋白病的黑质变性有关。低CDT-adj的iRBD患者更有可能表象转化为显性疾病。
原文出处:
Increased Transferrin Sialylation Predicts Phenoconversion in Isolated REM Sleep Behavior Disorder. Movement Disorders. Published online 2022:11.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#Disord#
106
#disorders#
115
#Dis#
75
#disorder#
84
#ERS#
88
#快速眼动睡眠#
0
#铁代谢#
96
#表型#
108