【一般资料】
患者女,78岁。
【主诉】
因“胸闷胸痛12天,黑色素瘤术后10年”入院。
【现病史】
10年前,左手拇指曾行“结节切除术”,病理证实“恶性黑色素瘤”,5年前因“心绞痛”行冠状动脉造影,未植入支架。
【体格检查】
前胸壁可见多个黑色结节,深入皮下,结节周围皮肤破溃出血,质韧,伴局部疼痛。心电图示房颤。
【辅助检查】
胸部CT显示:两肺及双侧胸膜可见散在多发大小不等结节状密度增高影,较大者位于右肺上叶、分叶状,大小约37mm×27mm,增强扫描呈轻度强化;胸壁皮下见多发结节影(图1)。腹部CT示:肝内多发结节样低密度影,边界欠清,增强扫描呈稍低环形强化,较大者直径约16mm。经胸超声心动图示:双房增大,右室心尖近室间隔处可见一偏高回声团,大小约19mm×19mm(图2),边界尚可辨,内部未见明显血流信号。首先考虑占位性病变。心脏声学造影:右室内可见充盈缺损,形态欠规整,周边于室间隔及右室壁分界不清,大小约2.1mm×15mm(图3),肿块增强与心肌无明显差异。



【治疗】
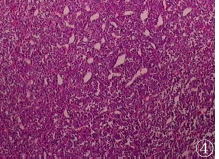
既往常规心脏超声未发现右室病变,可明确右室内为新发黑色素瘤转移灶。因患者较年长,一般情况较差,内科予以相应对症治疗,皮肤科对胸壁出血较多肿块行部分切除(图4),未进行进一步化疗等治疗,1周后自动出院。
【讨论】
恶性黑色素瘤是一种来源于恶性程度较高的产黑色素细胞的肿瘤,近年来发病率逐年升高,占皮肤恶性肿瘤的7%~20%,占所有恶性肿瘤的1%~2%。恶性黑色素瘤主要发病部位在皮肤,在生殖道、消化道、鼻腔等黏膜组织中较少发生。目前,黑色素瘤的病因未完全阐明,研究提示与遗传基因和环境刺激相关,如日照时间、人种及是否有家族史等因素。患者可早期发生血液及淋巴转移,恶性程度较大,较多累及肝、肺及肾上腺等器官,部分患者累及心脏。大部分转移性恶性黑色素瘤位于心肌内,可以累及心脏所有结构,右心系统更常见,心瓣膜非常少见。大部分患者发现心脏累及时,同时伴其他脏器累及,如本例患者合并肝、肺转移及胸壁多发转移。心脏声学造影应用于心脏占位的显示及鉴别,尤其是占位与心腔血栓鉴别。也有研究表明,心脏声学造影协助判断心脏占位性病变的性质,对比剂微泡在微循环的浓度代表该部位组织的血流灌注状况,外周静脉注射对比剂后,由于血栓的无滋养血管特性,在造影背景下,血栓显示出完全的充盈缺损,而肿瘤根据其良恶性不同、滋养血管多少的不同,表现出不同程度的对比剂增强特点。对于恶性肿瘤病史的患者,超声造影相对安全,无辐射,可以作为常规筛查手段。
原始出处:
程颖颖, 黄安茜, 包凌云. 恶性黑色素瘤右室转移1例[J]. 医学影像学杂志, 2017, 27(4):739-739.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#色素#
71
#黑色素#
83
#黑色素#
64
不错的文章值得拥有哦
96
关注
107