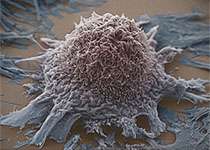
Blood:CSF1R抑制剂通过阻断支持细胞的旁分泌信号抑制急性髓系白血病细胞
2018-11-14 MedSci MedSci原创
中心点:CSF1R在支持细胞亚群中表达,其抑制可降低超过20%的AML患者样本的细胞活性。CSF1R活性刺激旁路细胞因子分泌,或可作为AML支持细胞的新治疗靶点。摘要:为明确AML的新的治疗靶点,研究人员对原发性AML患者样本进行小分子和siRNA筛选。在23%的样本中,研究人员发现了对CSF1R抑制的敏感性,CSF1R是一种受体酪氨酸激酶,调控髓系细胞的存活、增殖和分化。对CSF1R抑制剂GW-
CSF1R在支持细胞亚群中表达,其抑制可降低超过20%的AML患者样本的细胞活性。
CSF1R活性刺激旁路细胞因子分泌,或可作为AML支持细胞的新治疗靶点。
摘要:
为明确AML的新的治疗靶点,研究人员对原发性AML患者样本进行小分子和siRNA筛选。在23%的样本中,研究人员发现了对CSF1R抑制的敏感性,CSF1R是一种受体酪氨酸激酶,调控髓系细胞的存活、增殖和分化。对CSF1R抑制剂GW-2580的敏感性优先在新生和有利的风险患者中发现,对GW-2580耐受与整体生存率降低相关。
通过流式细胞术,研究人员发现CSF1R不是在大多数白血病细胞中表达,而是在支持细胞亚群中表达。通过大量细胞计数法(CyTOF)对比AML患者和健康供体的CSF1R表达细胞,结果发现CSF1R是独特的细胞表面标志物。
CSF1R表达细胞数量与GW-2580敏感性相关。将原发性AML患者样本暴露于一组重组细胞因子中,发现CSF1R抑制剂敏感性与对CSF1R配体、CSF1和其他细胞因子(包括HGF,另一种生长因子)的生长反应相关。添加CSF1可增加AML患者样本条件性培养基中HGF和其他细胞因子的分泌,加入GW-2580则可抑制其分泌。在未处理过的细胞中,HGF水平与GW-2580敏感性显著相关。最后,重组HGF和HS-5条件性培养基可恢复GW-2580处理过的AML患者样本的细胞活性。
综上所述,本研究表明CSF1R表达细胞通过分泌HGF和其他细胞因子来支持白血病细胞,提示CSF1R或可作为AML的新的治疗靶点,揭示了旁路细胞因子/生长因子分泌信号在该疾病中的作用机制。
David K. Edwards V,et al.CSF1R inhibitors exhibit anti-tumor activity in acute myeloid leukemia by blocking paracrine signals from support cells. Blood 2018 :blood-2018-03-838946; doi: https://doi.org/10.1182/blood-2018-03-838946
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#髓系白血病#
52
#支持细胞#
78
#阻断#
56
#分泌#
62
#CSF#
68
#抑制剂#
50
#CSF1#
74
#CSF1R#
63
#旁分泌#
74
学习
101