J Thromb Haemost:肝胆胰手术后内脏静脉血栓形成和死亡的发生率及预测因素
2020-12-02 MedSci原创 MedSci原创
30例肝胰胆管外科术后患者中平均有1例患者发生SVT,且其与90天死亡率增加3倍有关。
腹腔手术是内脏静脉血栓形成(SVT)已知的危险因素。肝胰胆外科手术后SVT的发生率、治疗和预后尚未明确。近日,血栓和凝血疾病权威杂志Journal of Thrombosis and Haemostasis上发表了一篇研究文章,这项研究旨在明确肝胰胆外科手术后SVT的发生率和预后,并描述术后SVT抗凝治疗的临床实践。

研究人员对接受肝胰胆管外科手术的成人进行了多中心回顾性队列研究。研究人员对SVT、大出血和90天死亡的预测因素进行了多变量分析。
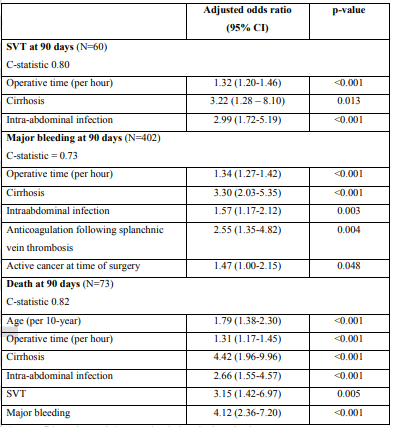
在1815例患者中,有89例(4.9%)患者伴有肝硬化,1532例(84.4%)患者伴有活动性癌症。最常见的手术是胰十二指肠切除术(40.6%)、开腹(30.7%)和腹腔镜(11.0%)肝切除术。60名(3.3%)患者在手术90天内经历了SVT。在SVT患者中,有症状的患者占23.3%,接受抗凝治疗的患者占75.0%。抗凝治疗持续时间平均为3-6个月。通过多变量分析,SVT的预测指标包括:手术时间(每增加1小时调整后的比值比[aOR]为1.32、95%CI为1.20-1.46)、肝硬化(aOR为3.22、95%CI为1.28-1.8.10)和术后腹腔内感染(aOR为2.99,95%CI为1.72-5.19)。22.1%的患者术后发生大出血,4.0%的患者在90天内死亡。术后死亡的预测因素包括:年龄(每增加10岁的aOR为1.79,95%CI为1.38-2.30)、手术时间(aOR为1.31(95%CI为1.17-1.45)、肝硬化(aOR为4.42、95%CI为1.96-9.96)、术后腹腔内感染(aOR为2.66,95%CI为1.55-4.57)、术后大出血(aOR为4.12,95%CI为2.36-7.30)和术后SVT(aOR为3.15,95%CI为1.42-6.97)。
由此可见,30例肝胰胆管外科术后患者中平均有1例患者发生SVT,且其与90天死亡率增加3倍有关。
原始出处:
Emmanuelle Duceppe.et al.Incidence and predictors of splanchnic vein thrombosis and mortality following hepatobiliary and pancreatic surgery.Journal of Thrombosis and Haemostasis.2020.https://onlinelibrary.wiley.com/doi/10.1111/jth.15198
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#静脉血#
40
#HAE#
42
#发生率#
50
#静脉#
40
#预测因素#
53
#静脉血栓形成#
0
🐂
78
好
96
不错
88
好
92