Nat Cell Biol:华人学者揭示卵巢癌治疗新策略
2017-07-31 佚名 药明康德
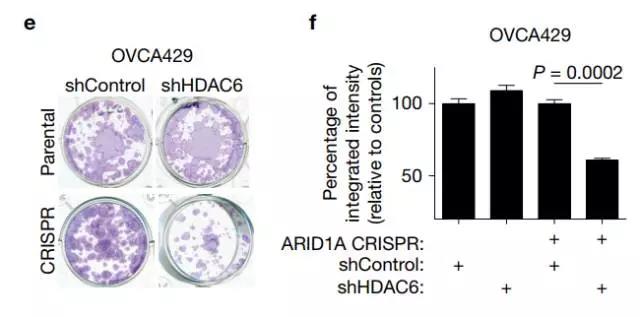
近日,我们不断看到华人学者们的亮眼表现:上周,《细胞》杂志同一期刊登了5篇来自华人学者的论文,占到了半壁江山。最近,美国宾夕法尼亚大学 / Wistar研究所的张如刚教授团队的一项研究又在线发表在了《自然》子刊《Nature Cell Biology》上,它对于卵巢癌新药的开发,有着极为重要的应用价值。


张如刚教授博士毕业于中国科学院上海生命科学研究院生物化学与细胞生物学研究所,并在宾夕法尼亚大学与Fox Chase癌症中心接受了博士后的训练。2012年,他加入了Wistar研究所。去年,他的工作被CDMRP评为年度卵巢癌研究的亮点之一。我们很高兴看到来自中国的学术新星能够在国际舞台上闪耀,也祝愿看到越来越多华人学者的身影。
19, 962–973 (2017) doi:10.1038/ncb3582
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Biol#
81
#治疗新策略#
79
#Nat#
97
#CEL#
67
#Cell#
66
#Bio#
68
#新策略#
67
#华人#
62
#华人学者#
78