Stroke:年龄改变来源不明栓塞性卒中患者左心房扩大和颈动脉非狭窄斑块的患病率
2022-04-02 MedSci原创 MedSci原创
年轻的ESUS患者患同侧非狭窄斑块的发生率较高,而老年人患LAE的发生率较高。在未来的研究中,应考虑年龄对ESUS特定机制的差异性影响。
非狭窄性颈动脉斑块和未检测到的房颤是不明源性栓塞卒中(ESUS)的潜在机制,但尚不清楚哪一种更可能是导致卒中的机制。近日,心血管疾病领域权威杂志Stroke上发表了一篇研究文章,研究人员旨在探讨ESUS人群中左心房扩大(LAE)和非狭窄性颈动脉斑块之间的关系。
研究人员对连续就诊的单侧前循环ESUS患者进行回顾性多中心队列调查(2015年至2021年)。LAE和斑块厚度分别由经胸超声心动图和计算机断层血管造影监测进行确定。研究人员描述性地统计比较了斑块特征与年龄和左心房尺寸之间的关系。
在接受筛查的4155名患者中,有273名(7%)患者符合纳入标准。中位年龄为65岁(四分位间距[IQR为54-74]),女性133例(48.7%),左房内径中位数为3.5cm(IQR为3.1-4.1)。任何LAE的患者更经常伴有高血压(85.9% vs. 67.2%,P<0.01)、糖尿病(41.0% vs. 25.6%,P=0.01)、血脂异常(56.4% vs. 40.0%,P=0.01)和冠状动脉疾病(22.8% vs. 11.3%,P=0.02)。
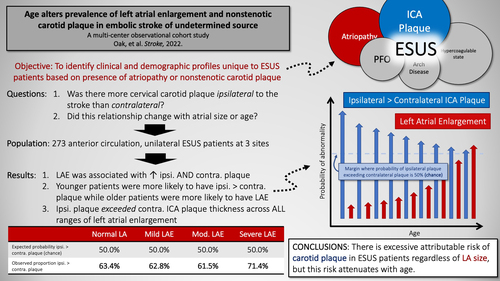
在整个队列中,与对侧相比,卒中半球同侧颈动脉斑块厚度更大(中位数为1.9mm[IQR为0-3]与1.5mm[IQR为0-2.6],P<0.01);然而,这在很大程度上是由没有LAE的亚组患者所驱动(中位数为1.8mm[IQR为0-2.9] vs. 1.5mm[IQR为0-2.5],P<0.01)。与年龄≥70岁的患者相比,年轻患者同侧颈动脉斑块多于对侧(平均差异为0.42mm±1.24 vs. 0.08mm±1.54,P=0.047),中度至重度LAE较少(6.3% vs. 15.3%,P=0.02)。
由此可见,年轻的ESUS患者患同侧非狭窄斑块的发生率较高,而老年人患LAE的发生率较高。在未来的研究中,应考虑年龄对ESUS特定机制的差异性影响。
原始出处:
Solomon Oak.et al.Age Alters Prevalence of Left Atrial Enlargement and Nonstenotic Carotid Plaque in Embolic Stroke of Undetermined Source.stroke.2022.https://www.ahajournals.org/doi/10.1161/STROKEAHA.121.037522
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#颈动脉#
68
#卒中患者#
70
#左心房#
82
#患病率#
80
#斑块#
97
#栓塞性卒中#
65
#心房#
74