Lancet:Meta分析:≥75岁老年人吃他汀也可获益
2019-03-30 xujing 中国循环杂志
据Lancet上发表的一项Meta分析,无论年龄大小,他汀类药物都能减少主要血管事件,包括75岁以上的老年人。
据Lancet上发表的一项Meta分析,无论年龄大小,他汀类药物都能减少主要血管事件,包括75岁以上的老年人。
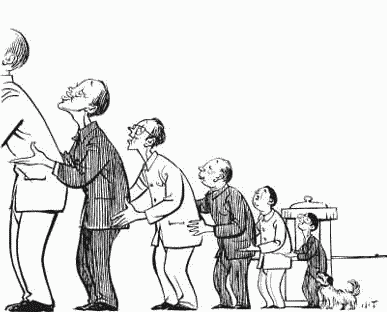
该分析纳入涉及13万多名22项他汀类药物治疗的随机对照试验以及涉及39612人的5项强化与非强化他汀类药物治疗的随机对照试验。分析了他汀在不同年龄组(55岁及以下、56~60岁、61~65岁、66~70岁、71~75岁、75岁以上)的疗效。
在4.9年的随访中,他汀类药物治疗可使低密度脂蛋白胆固醇降低1.0 mmol/L,进而主要血管事件降低21%。
所有年龄组的主要血管事件均显着减少,包括年龄大于75岁的14 483名受试者。但对于75岁以上的受试者,相对风险降低率略低(RR=0.87,尤其是在既往无血管疾病的人群(RR=0.92)。
他汀类药物治疗每降低1.0 mmol/L的低密度脂蛋白胆固醇,就可使主要冠状动脉事件的发生率降低24%,并且随着年龄的增长,主要冠状动脉事件发生率降低的趋势越来越小。
此外,使用他汀类药物每降低1.0 mmol/L的低密度脂蛋白胆固醇,所有年龄段冠状动脉血运重建手术的风险降低25%,卒中风险降低16%。
由于他汀类药物不能减少心衰或肾衰竭患者的心血管事件,因此在试验中纳入心脏或肾功能不全的老年受试者可能影响结果。
在排除4项仅纳入心力衰竭患者或接受肾透析患者的试验(其中他汀类药物治疗未被证明有效)后,随着年龄的增长,主要冠状动脉事件的风险降低趋势持续存在。
研究发现,每降低1.0 mmol/L的低密度脂蛋白胆固醇,血管死亡率就有12%的下降,随着年龄的增长,血管死亡率下降比例有减少的趋势。
他汀类药物治疗不影响任何年龄段的非血管性死亡率、癌症死亡或癌症发病率。
他汀类药物治疗常因多种原因而在老年患者中中断,例如伴随疾病和对风险-效益的认知。
原始出处:Cholesterol Treatment Trialists' Collaboration. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019 Feb 2;393(10170):407-415.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#MET#
93
#Lancet#
78
#Meta#
59
好
122
了解一下,谢谢分享!
123
学习了
123
谢谢分享学习
87