Dermatol Surg:这样治疗非黑素瘤皮肤癌是有效的
2016-08-04 Mechront 译 MedSci原创
根据最近的研究数据,使用激光烧蚀分数-局部氟尿嘧啶辅助治疗浅表基底细胞癌(BCC)和鳞状细胞原位癌(SCC)是有效的无创治疗手段。来自波士顿医疗中心皮肤科的Sarah H. Hsu博士和同事在以前的研究中发现了该治疗方式的短期疗效,但是长期结果仍未知。因此他们对30例原发性浅表型BCC或直径小于2cm的SCC患者使用了激光烧蚀分数和皮下外用5%的5-氟尿嘧啶7天。平均随访时间为15个月,26名患者
根据最近的研究数据,使用激光烧蚀分数-局部氟尿嘧啶辅助治疗浅表基底细胞癌(BCC)和鳞状细胞原位癌(SCC)是有效的无创治疗手段。
来自波士顿医疗中心皮肤科的Sarah H. Hsu博士和同事在以前的研究中发现了该治疗方式的短期疗效,但是长期结果仍未知。因此他们对30例原发性浅表型BCC或直径小于2cm的SCC患者使用了激光烧蚀分数和皮下外用5%的5-氟尿嘧啶7天。平均随访时间为15个月,26名患者中有20名在治疗4-8周时间里,进行了刮活组织检查,以验证组织间隙。
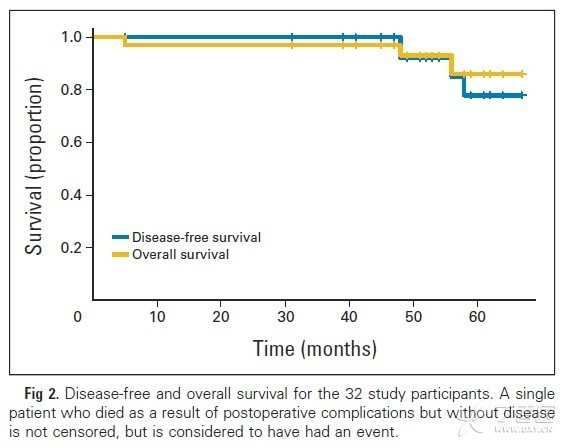
数据显示,总的治疗成功率为79%(95% CI,67-96)。SCC原位癌患者的成功率为92%,浅表BCC患者的成功率为67%。肿瘤位置或大小对治疗结果影响不显著。
研究人员写道,“大多数的治疗失败发生在治疗4-8周内,因此在一定程度上,可以通过治疗的初步反应预测长期的结果。随着人口老龄化,非黑素瘤皮肤癌的发生率增加,找到更加方便和符合成本效益的治疗方案是必要的,尤其是对复发低风险的浅表肿瘤。”
原始出处:
Ablative fractional laser with topical fluorouracil effective for some nonmelanoma skin cancers.Healio.August 3, 2016
Hsu S.H., et al. Ablative Fractional Laser-Assisted Topical Fluorouracil for the Treatment of Superficial Basal Cell Carcinoma and Squamous Cell Carcinoma In Situ: A Follow-Up Study..Dermatol Surg. 2016;doi:10.1097/DSS.0000000000000814.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#非黑素瘤皮肤癌#
76
#黑素瘤#
69
继续学习
0
继续关注
83