ASCO GU 2021: 免疫联合靶向在晚期肾癌中大获成功,完成2年治疗的人群结果公布(KEYNOTE-426研究)
2021-02-16 MedSci原创 MedSci原创
在过去的两年中,转移性肾细胞癌(mRCC)患者一线治疗的治疗方式发生了巨大变化。 2018年,CheckMate214数据的发布证明,在中度和低危mRCC中,与舒尼替尼相比,用nivolumab和ip
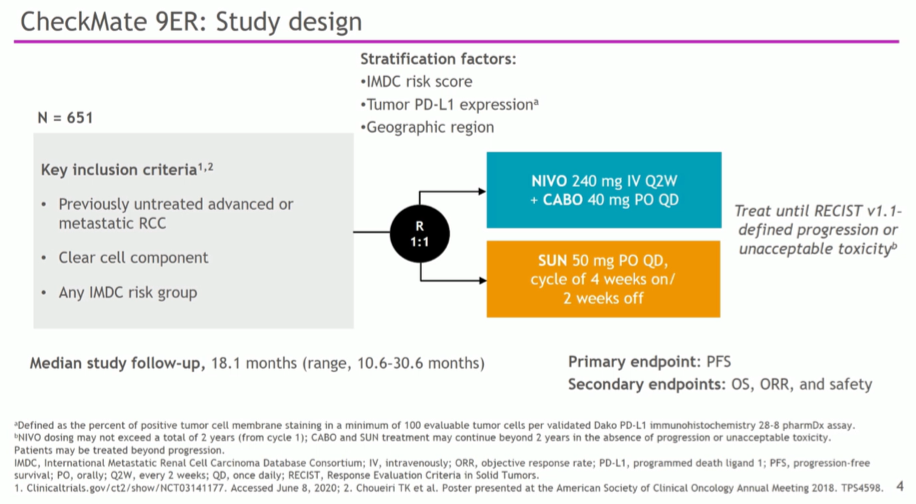
在过去的两年中,转移性肾细胞癌(mRCC)患者一线治疗的治疗方式发生了巨大变化。 2018年,CheckMate214数据的发布证明,在中度和低危mRCC中,与舒尼替尼相比,用nivolumab和ipilimumab治疗的患者具有生存优势,从而开启了mRCC的免疫治疗时代。随后发表的JAVELIN Renal 101,KEYNOTE-426和CheckMate-9ER研究证明了在这种疾病领域中,avelumab和axitinib,pembrolizumab和axitinib以及nivolumab和cabozantinib优于sunitinib(见:Lancet Oncol:派姆单抗联合阿西替尼治疗初治晚期肾癌的疗效优于单用舒尼替尼(Keynote-426))。在2021年美国临床肿瘤学会泌尿生殖系统癌症研讨会(ASCO GU)的海报重点会议:肾细胞癌-临床试验更新会议的全体会议摘要中,Plimack博士及其同事提供了KEYNOTE-426研究的最新进展接受派姆单抗和阿昔替尼治疗并已完成两年随访的患者的预后。长期随访结果也刚刚报道:Eur J Cancer:阿昔替尼联合派姆单抗治疗晚期肾癌的长期随访预后良好!
KEYNOTE-426研究共纳入861例接受一线治疗的晚期肾细胞癌患者,Karnofsky表现评分(KPS)≥70%,按1:1比例随机分配Pembrolizumab(200 mg 静脉注射 Q3W,最多35个周期)+axitinib(5mg 口服BID)(n= 432)或sunitinib治疗(50 mg口服QD,连续4周/停药2周)(n= 429),直至疾病进展、不能耐受毒性、研究者和患者决定停药等。按IMDC风险(有利vs中等vs较差)和地理区域(北美vs西欧vs世界其他地区)进行分层。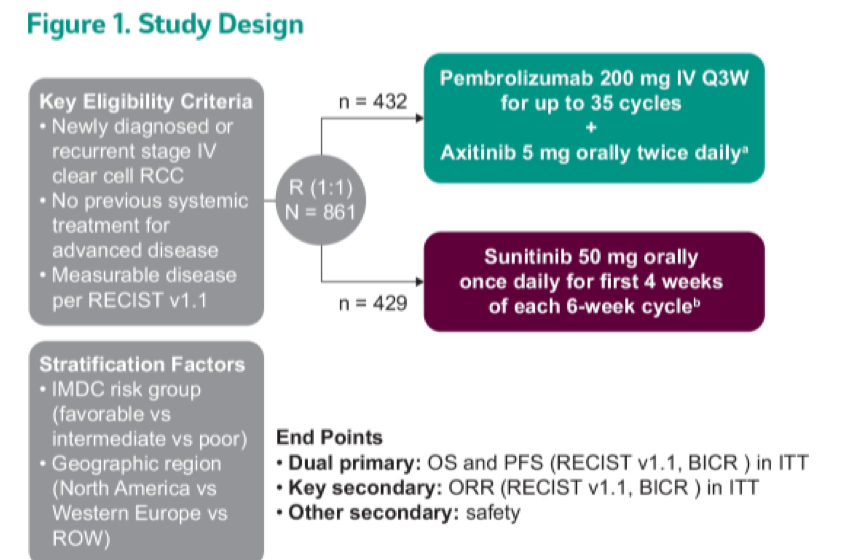
主要终点为总体生存期(OS)和无进展生存期(PFS),主要终点为客观缓解率(ORR)和安全性。 根据治疗方案,患者可以停用pembrolizumab或axitinib并继续使用其他药物。 所有患者均在2岁时停止使用Pembrolizumab。 阿昔替尼可以持续使用直至进展或出现毒性反应。
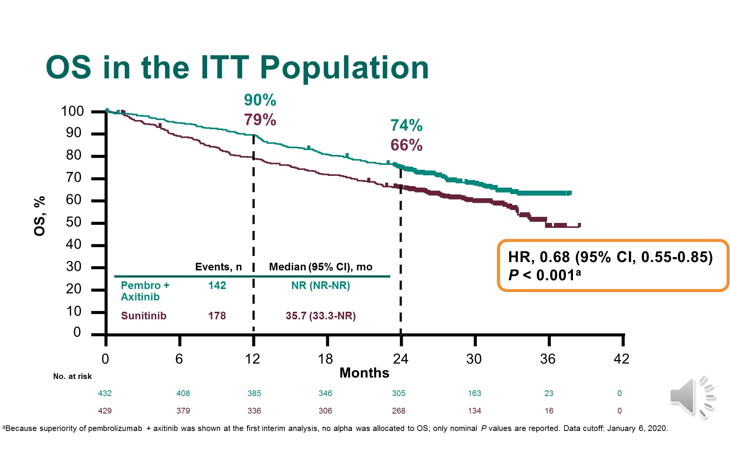
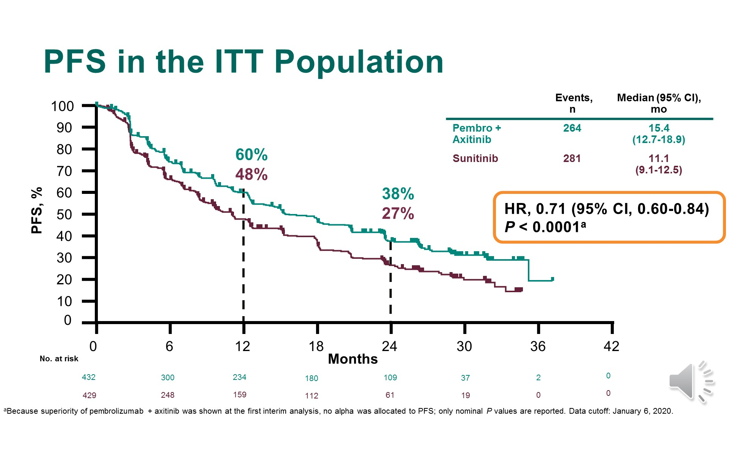
此前全人群的研究结果显示:帕博利珠单抗联合阿昔替尼较舒尼替尼可明显改善OS[HR=0.68(95% CI:0.55~0.85);P<0.001];24个月OS率分别为74%和66%。帕博利珠单抗+阿昔替尼组和舒尼替尼组的中位OS分别为未达到和35.7个月。帕博利珠单抗联合阿昔替尼较舒尼替尼明显改善了PFS,两组中位PFS分别为15.4个月和11.1个月(HR=0.71,P<0.001), 24个月PFS率分别为38%和27%。
在本次报告中,作者报告了KEYNOTE-426的探索性亚组分析,即完成2年帕博利珠单抗治疗的患者的结局。
在432例接受pembrolizumab和axitinib治疗的患者中,有129名(29.9%)完成了2年的研究治疗。 作者进一步将分析限制在103名因进行性疾病而未停用阿昔替尼的患者中。 这些患者的中位(范围)年龄为61(36-82)岁,男性为73.8%。
此子集中的大多数患者患有国际mRCC数据库联合会的中度/低危疾病(n = 67),而36例患有有利风险的疾病,与意向治疗人群一致。
从随机分组到数据截止的中位(范围)随访时间为30.1(24.0-37.7)个月。 在完成2年研究治疗的患者中,截至3年,均未达到中位总体生存率或中位无进展生存率。
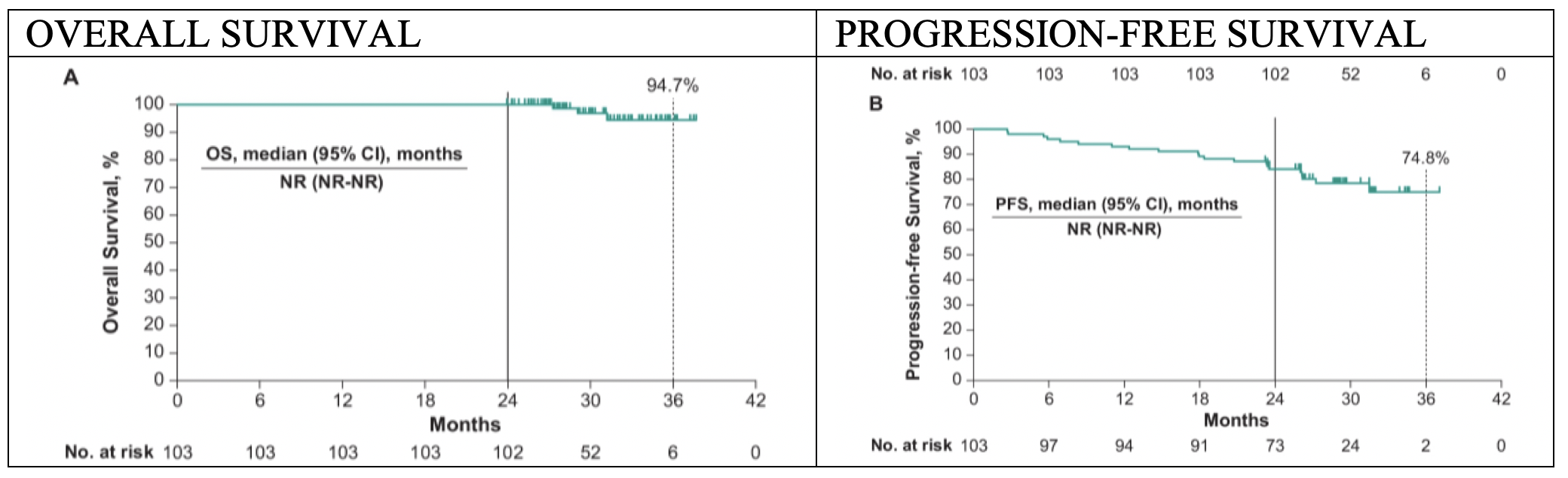
按照方案完成两年治疗的患者中,有85.4%的患者有客观反应,其中16例患者有完全反应。
在多变量分析中,年龄小于65岁的患者(OR 1.76,95%CI 1.07-2.90),表现状态为90/100(OR 2.10,95%CI 1.03-4.24),良好(OR 4.99,95%)的患者 CI为1.63-15.27)和中度(OR 4.90,95%CI 1.67-14.41)的危险疾病以及具有肉瘤样特征的患者(OR 2.19,95%CI 1.08-4.43)更有可能完成两年的治疗。 60.2%的患者经历了与3-4级治疗相关的不良事件,而没有任何5级事件。
这项探索性分析表明,pembrolizumab和axitinib组中的很大一部分患者能够完成2年的pembrolizumab治疗,并具有持续的临床获益。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#KEYNOTE#
98
#联合靶向#
76
#ASC#
73
#结果公布#
82
#晚期肾癌#
107