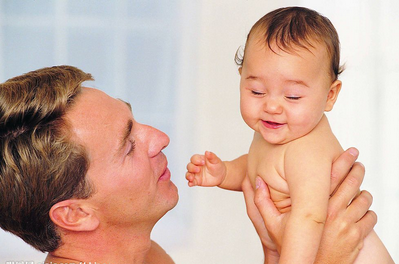
J Affect Disord:不会吧?爸爸们也会得产后抑郁症?
2015-11-27 陈说 译 MedSci原创
根据情感障碍杂志发表的一项研究显示,父亲们在一个新生婴儿的到来过程中可能会出现焦虑症。
近日,情感障碍杂志上最新发表的一项研究结果表明,在迎接一个新生婴儿到来的过程中,男人也会出现产后抑郁症。
以往的研究发现,超过20%的父母在产后患上了焦虑和抑郁。而对于新生婴儿的到来,导致父母们出现焦虑和抑郁的原因,人们目前还知之甚少。
该研究设计的研究数据主要包含两个---产后男性焦虑症状和患病率(孩子出生前以及出生后的第一年)。
研究结果发现,不管是孩子出生前还是出生后,男性普遍会出现抑郁症状,大约10名男子中就有1位出现症状,概率约为女性患抑郁症的一半。此外,孩子出生前男性出现抑郁的概率为4.1%和16%之间,出生后为2.4%至18%。
对于是何种风险因素导致男性出现产后抑郁,主要因素可以归结为缺乏社会支持,特别是从合作伙伴,财政困难和精神健康问题等方面。另外,CDC认为,15-24岁以及那些低教育程度和收入都较低的父亲最有可能经历抑郁。
当男性出现焦虑症的症状可能表现为精神紧张、烦躁和担忧婴儿的安全等等。有时还会出现手心出汗、睡眠差和食欲下降等现象。
Leach博士说:
“当一个新生婴儿的降临时,对于很多父母来说需要一段时间来进行自身的调整,有时出现少许紧张属于正常的现象。但若出现焦虑,并持续时间较长且影响到日常生活,这时就得注意了。”
Leach博士还说,大多数情况下男性在女性怀孕和分娩的整个过程中可能会感到被排除在外,毕竟在整个怀孕和分娩过程中女性才是最重要的主角。她补充道,在这个时候,医疗保健的范围应该涉及整个家庭,无论是产科或是精神健康方面,并呼吁夫妇们意识到他们怀孕时要时刻关注自己的心里健康。
另外,Leach博士还指出,通常男性在刚开始出现焦虑症状时很少向他人寻求帮助,他们通常认为这对自己来说不算什么。但事实上正相反,他们应该寻求帮助,因为早期干预可以减少症状程度的加重和持续时间。如果他们不这样做,他们的焦虑不仅会对自己造成不利影响,同时还会对他们的妻子甚至是孩子有不良的影响。
Liana S. Leach et al., Prevalence and course of anxiety disorders (and symptom levels) in men across the perinatal period: A systematic review, Journal of Affective Disorders 24 November 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Dis#
64
#Affect#
99
#Disord#
70
以前没想到,今后注意这个问题
221
#产后抑郁#
79