喜大普奔!中国原创方案突破白血病世界性难题
2016-11-14 佚名 新华社
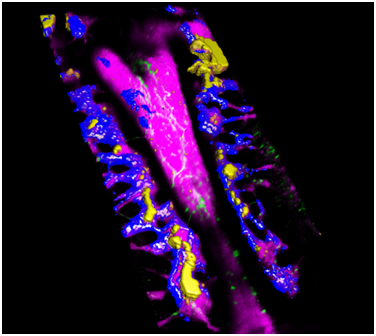
13日在京闭幕的第七届亚洲细胞治疗组织年会上,与会各国专家肯定了该方案对全球作出的贡献。作为一种恶性血液疾病,白血病的死亡率占儿童恶性疾病死亡率的第一位、成人恶性疾病死亡率的第六位。治疗该病的最有效方法是进行造血干细胞移植即骨髓移植。然而,骨髓移植须在人类白细胞抗原(HLA)100%全相合的情况下进行,否则极易发生严重排异反应。但即使是同胞兄妹,全相合概率也仅有25%,而没有血缘关系的人群,全相合
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














收藏
139
很好,不错,以后会多学习
129
棒哒哒
129
喜大普奔
129
喜大普奔
133
骄傲
85