JTO: SCLC预防性脑照射伴或不伴海马保护的3期随机试验
2021-04-29 MedSci原创 MedSci原创
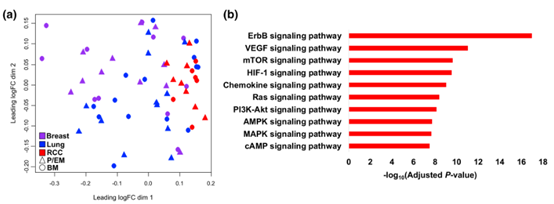
根据疾病分期及特征,小细胞肺癌患者的脑转移(brain metastases,BM)发生率非常高,超过50%。BM患者预后不佳,生活质量下降。
根据疾病分期及特征,小细胞肺癌患者的脑转移(brain metastases,BM)发生率非常高,超过50%。BM患者预后不佳,生活质量下降。预防性脑照射(phylactic cranial irradiation,PCI)可显著降低BM,并在一定程度上提高总生存率(OS)。但PCI会产生副作用,其中包括长期的神经认知功能下降。

目前,有研究已经提出了几种解释神经认知衰退的相互作用机制,其中包括血管病变、少突胶质细胞减少、中枢神经系统炎症和海马体中祖细胞生态退化,而海马体是学习和记忆的重要结构。海马功能受PCI影响最大。
现代放射治疗技术,如调强适形放射治疗和容积弧形调强放射治疗,允许以标准放射剂量治疗整个大脑但同时保持对海马的低剂量照射。本研究是一项多中心随机3期试验,旨在探讨比较小细胞肺癌患者接受PCI加或不加海马保护(hippocampus avoidance,HA)后的神经认知功能。
本研究将小细胞肺癌患者随机分为2组,接受剂量为2.5Gy*10f的标准PCI或HA-PCI治疗。主要终点是在4个月时测试霍普金斯词汇学习测验-修订版,如果与基线相比至少下降5个点则被视为失败。次要终点包括其他认知结果、发病率评估、脑转移位置和总生存率。
表1 所有接受HA-PCI治疗患者的治疗计划

在2013年4月至2018年3月,本研究共随机入组168名患者。中位随访时间为26.6个月。在两个治疗组中,70%的患者疾病有限,基线特征良好。在4个月时测定的霍普金斯词汇学习测验-修订版总回忆评分的下降在两组之间没有显著差异:29%接受PCI治疗的患者和28%接受HA-PCI治疗的患者下降大于或等于5分(p =1.000)。
在其他认知测试如测试记忆、执行功能、注意力、运动功能和处理速度的表现在两组之间没有显著差异。总生存率无显著性差异(p = 0.43)。PCI组2年的脑转移累积发生率为20%(95%CI:12%-29%),HA-PCI组为16%(95%CI:7%-24%)。
综上所述,本研究结果表明,与传统的PCI相比,小细胞肺癌患者接受HA-PCI的神经认知功能下降的概率并未发现有所减低。
Belderbos, José S.A. et al. Phase 3 Randomized Trial of Prophylactic Cranial Irradiation With or Without Hippocampus Avoidance in SCLC (NCT01780675). Journal of Thoracic Oncology, Volume 16, Issue 5, 840 - 849
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#预防性#
120
#随机试验#
95
#JTO#点击进入话题查看更多相关文章 或评论时插入话题加入讨论
101
高质量研究,读起来真爽,谢谢梅斯
87