Eur Urol Focus:机器人肾部分切除术后的并发症预测:回归简单
2021-05-30 AlexYang MedSci原创
机器人肾部分切除术(RPN)是治疗小肾脏肿瘤(SRTs)的一个推荐治疗选择,该治疗方法能提供最佳的肿瘤治疗效果。然而,即使有了丰富的手术经验,RPN仍然是一个复杂的、技术要求很高的手术。
机器人肾部分切除术(RPN)是治疗小肾脏肿瘤(SRTs)的一个推荐治疗选择,该治疗方法能提供最佳的肿瘤治疗效果。然而,即使有了丰富的手术经验,RPN仍然是一个复杂的、技术要求很高的手术。

机器人肾部分切除术(RPN)的发病率很高。肾功能评分已用于预测并发症的发生。但其实用性尚有争议。
近期,有研究人员评估了三种肾功能评分(RENAL、PADUA和SPARE)在预测围手术期结果的临床效用,并将其效果与进行简单测量肿瘤大小的预测效果进行比较,研究的队列是进行RPN的大队列。
他们共分析了1581名因小肾脏肿块而接受RPN的连续患者。根据术前成像计算了肿瘤大小、RENAL、PADUA和SPARE评分。评估了评分、估计失血量(EBL)、手术时间(OT)和热缺血时间(WIT)之间的相关性。研究人员利用逻辑回归分析确定总的和主要并发症的预测因素。曲线下的面积用来确定具有最高区分度的模型。决策曲线分析确定了相关的净收益。参与群体的中位年龄为62岁(四分位数范围[IQR]:52-70),中位肿瘤大小为35毫米(IQR:25-47)。结果发现,346名患者(21.9%)出现了术后并发症,5.6%的为主要并发症。所有评分都与EBL、OT和WIT显著相关。然而,关联性较弱,相关系数均<0.3。在单变量和调整后的多变量逻辑回归模型分析中,肾功能评分和肿瘤大小是总体并发症的重要预测因素。然而,决策曲线分析显示,肿瘤大小的净收益与所有肾功能评分分数相当。最后,他们发现肾功能评分和肿瘤大小都与主要并发症的风险无关。
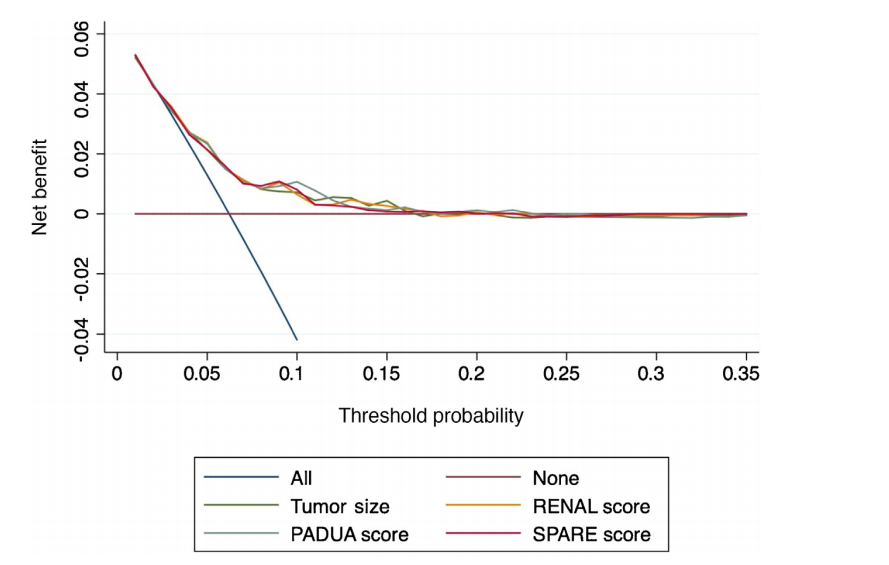
肿瘤大小和肾功能评分在预测主要并发症中的临床净益处
综上所述,肿瘤大小具有与肾功能评分分数相当的预测RPN围手术期结果的能力。
原始出处:
Zine-Eddine Khene, Clément Mazouin, Alessandro Larcher et al. Predicting Complications After Robotic Partial Nephrectomy: Back to Simplicity. Eur Urol Focus. May 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#切除术#
82
#并发#
86
#机器人#
96
#机器#
94
好文章,长知识
128