EUR J Cancer:帕尼单抗联合顺铂/吉西他滨治疗KRAS野生型胆管癌
2018-02-28 MedSci MedSci原创
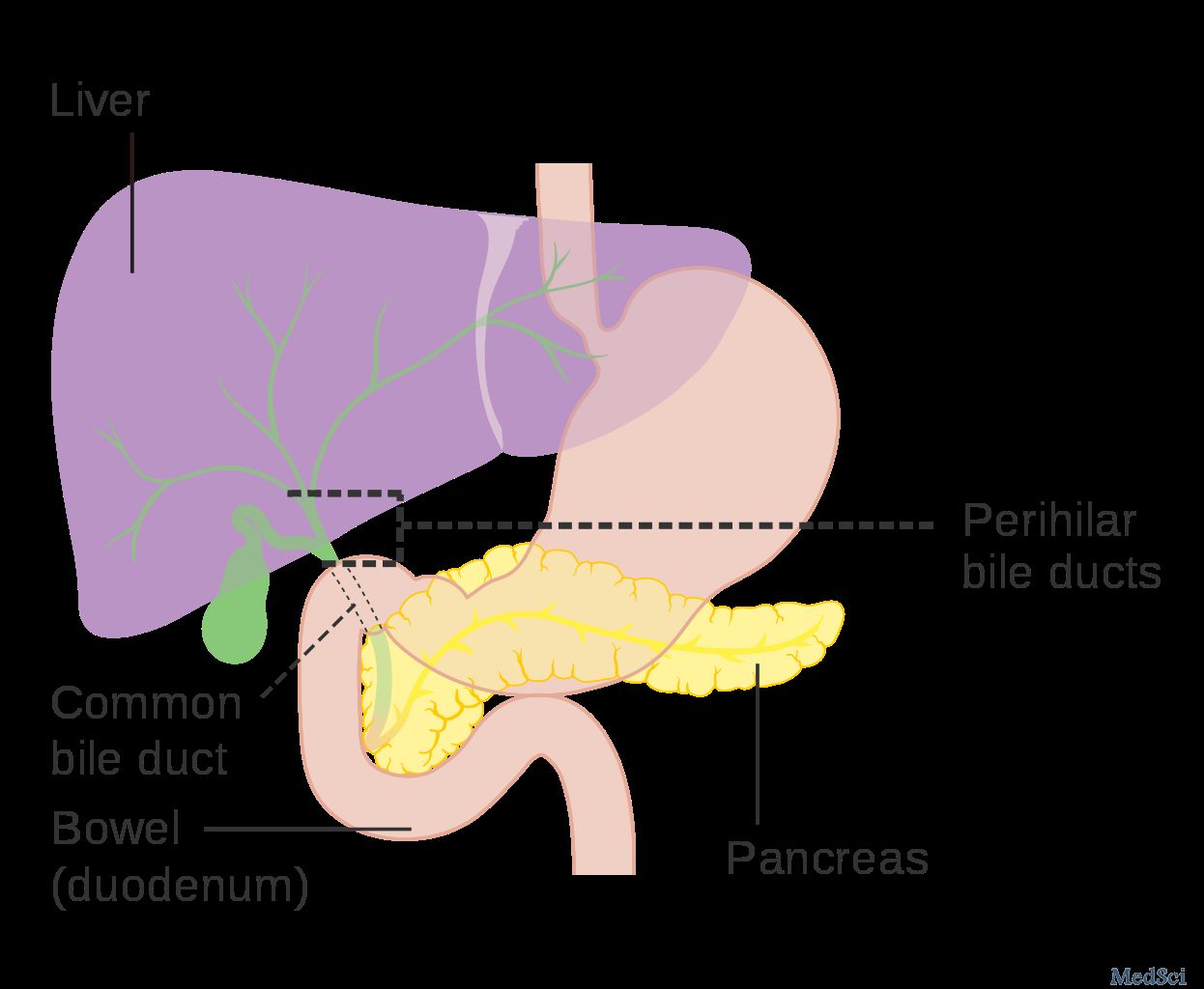
联合化疗已显示出在胆管癌治疗方面的优势,并且通过添加生物制剂可以实现进一步的改善。研究人员在此报道称EGFR抗体帕尼单抗在KRAS野生型胆管癌治疗的效果。
EUR J Cancer:帕尼单抗联合顺铂/吉西他滨治疗KRAS野生型胆管癌
联合化疗已显示出在胆管癌治疗方面的优势,并且通过添加生物制剂可以实现进一步的改善。研究人员在此报道称EGFR抗体帕尼单抗在KRAS野生型胆管癌治疗的效果。
晚期胆管癌患者被随机分配(2:1),第1天和第8天使用(A组,62例患者)或不使用帕尼单抗(B组,28例患者),同时接受顺铂(25 mg / m2)和吉西他滨联合化疗,主要终点为6个月时的无进展生存期(PFS)。次要终点包括客观缓解率(ORR),总生存率(OS)和毒性。此外,研究人员还对使用和不使用EGFR抗体的化疗结果进行了荟萃分析。
用顺铂/吉西他滨/帕尼单抗治疗的患者在6个月时的PFS率为54%,而顺铂/吉西他滨组为73%。 次要终点:A组的ORR为45%,B组为39%,中位OS分别为12.8个月(A组)和20.1个月(B组)。根据研究结果,12项试验的荟萃分析并未显示EGFR抗体治疗组与单纯化疗组的优势。
因此,帕尼单抗联合化疗并不能改善KRAS野生型晚期胆管癌患者的ORR,PFS和OS。
原始出处:
Vogel,
Arndt, et al. "PICCA study: panitumumab in combination with
cisplatin/gemcitabine chemotherapy in KRAS wild-type patients with biliary
cancer-a randomised biomarker-driven clinical phase II AIO study."
European Journal of Cancer 2018 92: 11-19. doi.org/10.1016/j.ejca.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#野生型#
68
#铂#
68
#KRAS#
67
#帕尼单抗#
83
#胆管#
69