葛均波院士牵头奥美沙坦酯氨氯地平片真实世界研究在沪启动!
2019-07-31 Fiona MedSci原创
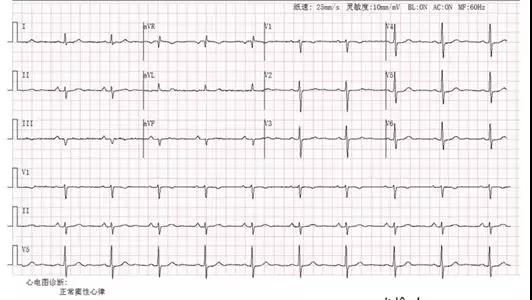
2019年7月31日,由复旦大学附属中山医院葛均波院士牵头的《奥美沙坦酯氨氯地平片对于中国原发性高血压人群的临床效果和安全性的多中心观察性研究》研讨会在上海正式拉开帷幕。复旦大学附属中山医院葛均波院士、复旦大学附属中山医院崔兆强教授、第一三共株式会社Head of ASCA MA东山浩先生、第一三共(中国)投资有限公司医学部总监张莹女士及中国心血管健康联盟医学部等共同出席了会议。葛均波院士表示,《



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#奥美沙坦#
71
#真实世界#
70
#氨氯地平#
93
#葛均波院士#
76
院士是学术至高点,也是大家必争之地呀
96