Gut:家族性胰腺癌高危个体可50岁启动MRI联合EUS筛查
2016-06-04 高晓方 翻译 中国医学论坛报
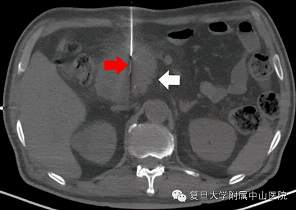
欧洲一项研究表明,在非CDKN2A基因突变的家族性胰腺癌(FPC)高危个体中,50岁启动胰腺导管腺癌筛查具安全性;MRI辅以超声内镜(EUS,基线时、每3年1次或MRI提示病变变化时)的筛查具有效性。论文5月24日在线发表于《消化道》(Gut)杂志。该研究纳入253例中位年龄48岁、非CDKN2A基因突变的FPC高危个体,给予MRI和EUS筛查。中位随访28个月。分析年龄和不同筛查方案的病变检出率
欧洲一项研究表明,在非CDKN2A基因突变的家族性胰腺癌(FPC)高危个体中,50岁启动胰腺导管腺癌筛查具安全性;MRI辅以超声内镜(EUS,基线时、每3年1次或MRI提示病变变化时)的筛查具有效性。论文5月24日在线发表于《消化道》(Gut)杂志。
该研究纳入253例中位年龄48岁、非CDKN2A基因突变的FPC高危个体,给予MRI和EUS筛查。中位随访28个月。分析年龄和不同筛查方案的病变检出率。
结果显示,中位筛查3次。基线或筛查中发现影像学胰腺病变为134例(53%),主要为胰腺囊肿(94%)。年龄≥45岁的受试者胰腺病变检出率显著升高。21例接受手术的受试者中,在50岁前检出了非显著性病变。在50岁后受试者潜在相关性病变的发生率显著升高。每年MRI联合EUS或每年MRI联合每3年1次EUS筛查在潜在相关性病变检出率方面无显著差异,且在筛查间期12个月和≥24个月的病变检出率亦无显著差异。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#EUS#
67
#家族性#
0
不错的文章,多学习
157
不错的文章,多学习
144
不错的文章,多学习
143