系统性红斑狼疮活性和羟氯喹在终末期肾病前后的使用情况
2022-09-18 August MedSci原创 发表于上海
狼疮相关终末期肾病 (ESRD) 是狼疮肾炎 (LN) 最常见的并发症。
狼疮相关终末期肾病 (ESRD) 是狼疮肾炎 (LN) 最常见的并发症。系统性红斑狼疮 (SLE) 相关 ESRD 患者的估计死亡率是单独 LN 的 SLE 患者的四倍,是非 SLE ESRD 患者的两倍。ESRD 后的 SLE 表现可能未被充分诊断和治疗,导致发病率和死亡率增加。诊断 ESRD 后活动性 SLE 是一项重大挑战。先前的研究表明,即使在进展为 ESRD 之后,SLE 活动仍会持续存在。目前,没有关于如何在 ESRD 后管理 SLE 相关药物的循证指南。了解 HCQ 处方模式和相关因素是确定可能受益于持续 HCQ 的患者的必要的第一步,最终目标是改善某些患者的结果,同时减少其他患者的不必要暴露和毒性。
ESRD 前后的临床和血清学 SLE 表现(N = 59):

研究目的:1) 评估临床和血清学 SLE 活动如何在 ESRD 前后演变和 2) 研究可能影响 ESRD 后 HCQ 处方的因素。从这项研究中获得的知识可能有助于识别 ESRD 后的 SLE 表现和 HCQ 使用情况。
方法:对 2010 年至 2017 年期间发生 ESRD 的 SLE 患者进行了一项回顾性队列研究。从 ESRD 发展前后的医疗记录中收集了 SLE 相关症状、疾病活动的血清学标志物和药物使用情况。
ESRD 诊断后基线人口统计学和临床/血清学 SLE 表现与使用 HCQ的比较:
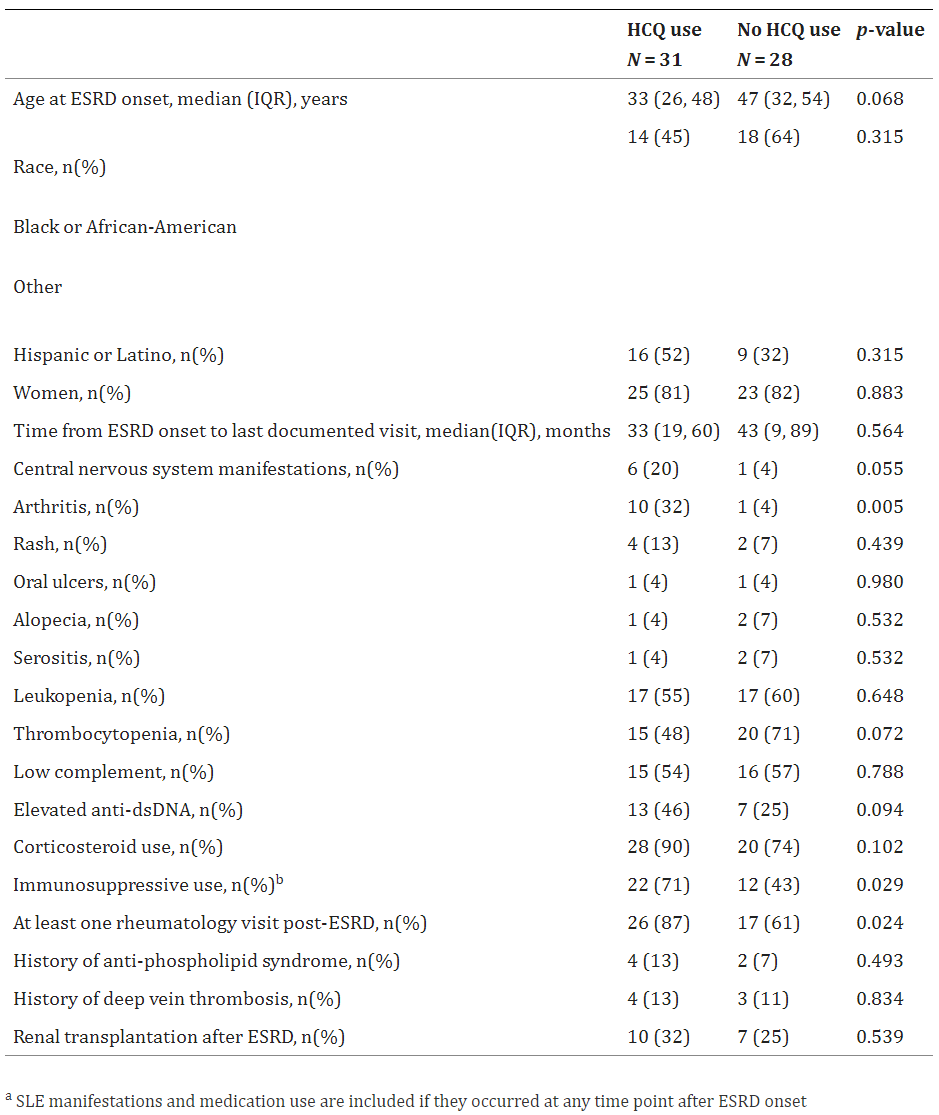
结果:59 名患者被纳入研究。25 名 (43%) 患者在 ESRD 前 12 个月内记录了至少一种临床(非肾脏)SLE 表现。其中,11/25 (44%) 在 ESRD 后继续出现狼疮症状;9 名在 ESRD 前没有临床或血清学活动的患者出现了活动性 SLE 的新症状。在 ESRD 后最后一次记录的访视中,42/59 (71%) 的患者有一个或多个狼疮活动的临床或血清学标志物;只有 17/59 (29%) 的患者达到临床和血清学缓解。
59 名患者中有 33 名 (56%) 在 ESRD 时有有效的 HCQ 处方。在 ESRD 后出现活动性 SLE 表现的 42 名 (62%) 患者中,有 26 名使用 HCQ。ESRD 后继续使用 HCQ 的患者更有可能接受风湿病专家的随访(26 [87%] vs 17 [61%],p = 0.024),记录的关节炎频率更高(10 [32%] vs 1 [ 4%],p = 0.005),CNS 表现(6 [20%] vs 1 [4%],p = 0.055)和同时使用免疫抑制药物(22 [71%] vs 12 [43%],p = 0.029 )。
综上所述,狼疮活动可能在 ESRD 发展后持续存在。可能会出现新发关节炎、狼疮相关皮疹、CNS 表现、低补体和抗 dsDNA 升高。在 ESRD 前后有活动性疾病证据的患者中,HCQ 可能未得到充分利用。建议对 SLE 患者在 ESRD 前后进行仔细的临床和血清学监测,以发现活动性疾病的迹象和频繁的风湿病学随访。
参考文献:Salgado Guerrero M, Londono Jimenez A, Dobrowolski C, Mowrey WB, Goilav B, Wang S, Broder A. Systemic lupus Erythematosus activity and Hydroxychloroquine use before and after end-stage renal disease. BMC Nephrol. 2020 Oct 28;21(1):450. doi: 10.1186/s12882-020-02083-2. PMID: 33115441; PMCID: PMC7592532.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#终末期#
82
#使用情况#
89
#系统性#
75
感谢分享
87
#狼疮#
150
#红斑#
83
#终末期肾病#
67