Cell:会不会感染轮状病毒原来是由肠道细菌决定的?
2019-10-19 不详 生物探索
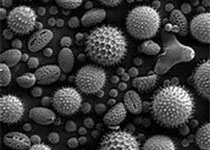
轮状病毒是一种具有高度传染性的病毒,可引起严重的腹泻、呕吐、发烧、腹痛和死亡。轮状病毒感染是由于直接与感染者接触或接触其粪便而发生的。婴儿和幼儿最容易感染这种疾病,这种疾病可能导致严重的脱水甚至死亡。根据疾病控制和预防中心的数据,全世界每年因感染轮状病毒而死亡的5岁以下儿童约为21.5万人。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














学习
31
#CEL#
39
#Cell#
33
#肠道细菌#
0
#轮状病毒#
43