Eur Urol:机器人辅助前列腺根治术中使用新型尿道固定技术与标准膀胱尿道吻合术的比较
2021-02-24 AlexYang MedSci原创
即使在机器人时代,前列腺根治性切除术后的尿失禁恢复仍旧是一个重大问题。人们也在不断的探索旨在改善更早恢复尿失禁的手术技术。最近,有研究人员描述了在机器人辅助根治性前列腺切除术(RARP)中新的尿道固定
即使在机器人时代,前列腺根治性切除术后的尿失禁恢复仍旧是一个重大问题。人们也在不断的探索旨在改善更早恢复尿失禁的手术技术。最近,有研究人员描述了在机器人辅助根治性前列腺切除术(RARP)中新的尿道固定手术技术 ,并评估了早期尿失禁恢复情况和围手术期并发症情况。
研究人员对2019年1月至12月期间接受RARP的70名连续患者进行了分析,并对研究组的35名接受尿道固定技术手术的患者与对照组的35名接受标准膀胱尿道吻合术的患者进行比较。结果表明,两组在所有的人口统计学、临床和病理学变量方面均相当。研究组34名(97.1%)患者和对照组28名(80%)患者在拔除导尿管后3个月恢复尿失禁(P=0.02)。与对照组相比,研究组患者在拔除导尿管后1周和1个月也具有较高的尿失禁率(分别为68.6% vs 45.7%,p=0.04;80% vs 54.3%,p=0.04)。手术室时间(p=0.7)或估计失血量(p=0.65)没有观察到差异。研究组中1名(2.9%)患者和对照组4名(11.4%)患者观察到90天的术后并发症(p=0.3)。主要的局限性是对相对较小的队列进行非随机比较。
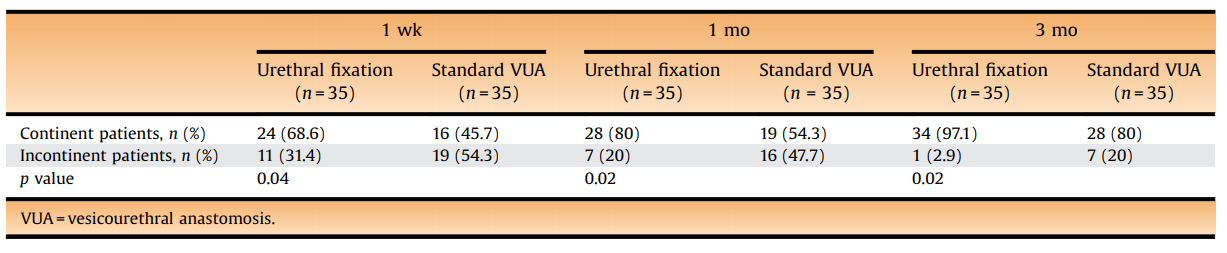
最后,研究人员指出,他们观察到在RARP期间,使用新型尿道固定技术与标准膀胱尿道吻合术相比,早期尿失禁恢复有显著改善,且手术室时间或围手术期并发症没有增加。
原始出处:
Vincenzo Ficarra , Marta Rossanese , Alessandro Crestani et al. Robot-assisted Radical Prostatectomy Using the Novel Urethral Fixation Technique Versus Standard Vesicourethral Anastomosis. Eur Urol. Feb 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#尿道#
113
#吻合术#
82
#机器人#
0
#根治术#
126
#机器人辅助#
88
#机器#
85
#根治#
165