Sci Transl Med:避无可避!炎症竟成皮肤癌“真凶”,该重视起来了!
2018-08-26 Paris,Zoe 转化医学网
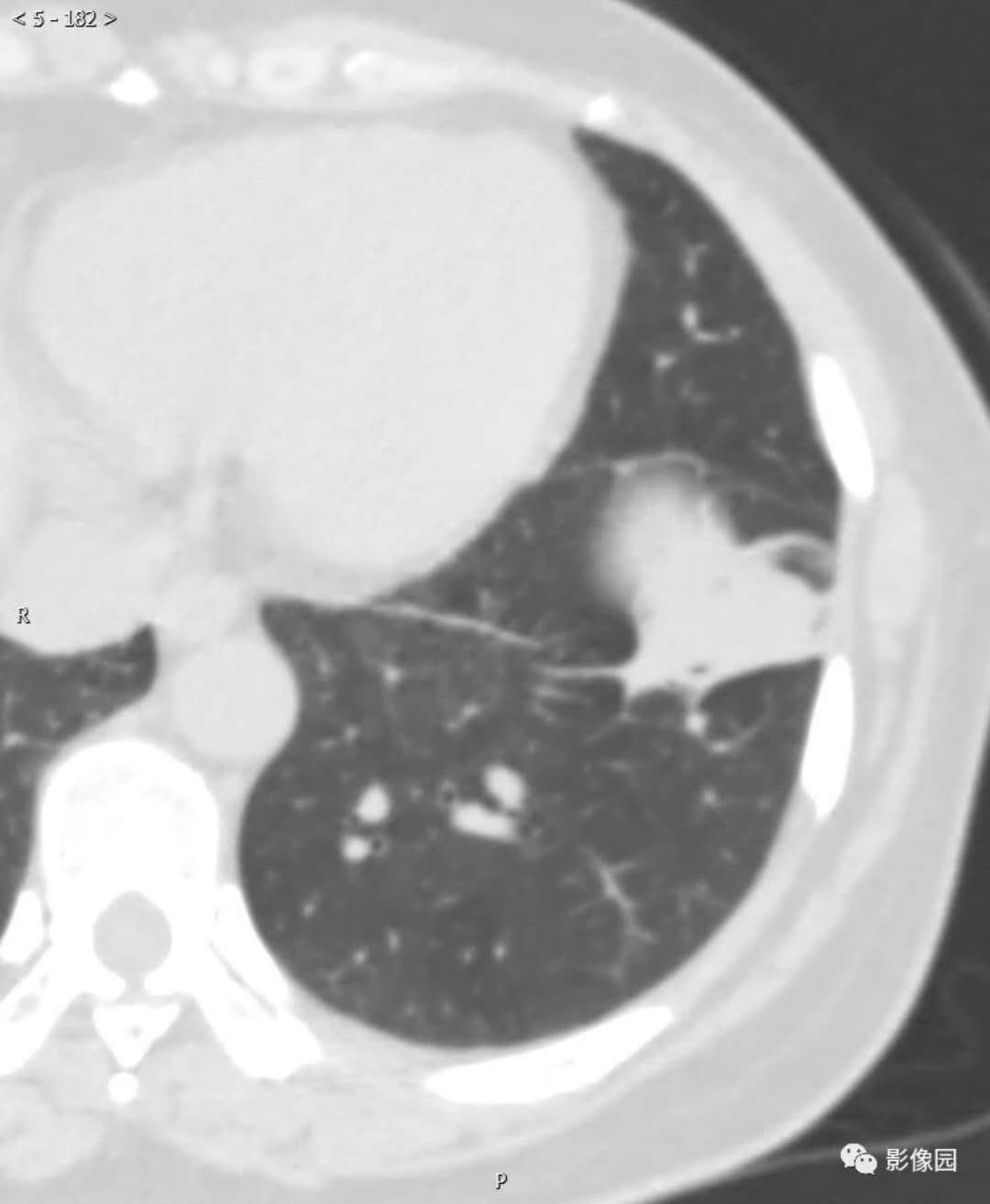
有研究表明,皮肤癌发病与日光照射、电离辐射损伤、接触化学制品、病毒和灼伤等因素相关,其中长期暴露在太阳紫外线下会导致DNA突变,进而发展为皮肤癌。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TRA#
56
#Transl#
54
#Med#
81
学习了谢谢
89
炎症和皮肤癌有关。
89
学习了,涨知识了!
110