NEJM:抑制雌激素可提高绝经前乳腺癌患者预后
2014-12-30 MedSci MedSci原创
Figure 1. Randomization and Primary Analysis Populations. Figure 2. Primary Analysis Comparisons of Tamoxifen plus Ovarian Suppression (OS) with Tamoxifen Alone. 抑制卵巢雌激素产生可降低激素受体阳性的绝经前妇女早期乳腺癌复发率
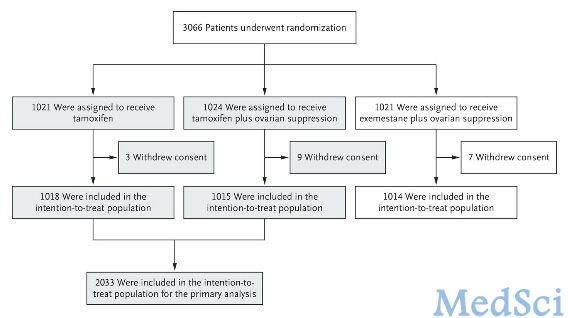
Figure 1. Randomization and Primary Analysis Populations.
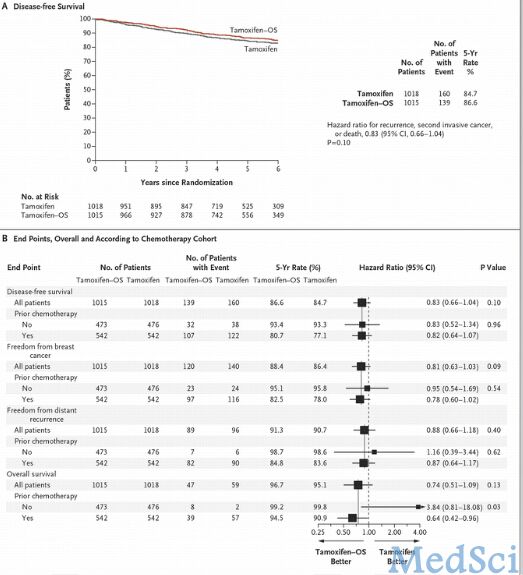
Figure 2. Primary Analysis Comparisons of Tamoxifen plus Ovarian Suppression (OS) with Tamoxifen Alone.
抑制卵巢雌激素产生可降低激素受体阳性的绝经前妇女早期乳腺癌复发率,但是否加入他莫昔芬尚无确切定论。
我们选取3066名绝经前妇女,根据有或无化疗收据纳入,分为接受5年他莫昔芬治疗、他莫昔芬辅助卵巢功能抑制治疗,以及依西美坦辅助卵巢功能抑制治疗组。验证假说,与单独给予他莫昔芬治疗相比,采用他莫昔芬辅助卵巢抑制治疗将提高无病生存率。受试对象中有46.7%没有接受过化学治疗,53.3%接受过化学治疗并且为绝经前妇女。
在平均随访67个月后显示,他莫昔芬辅助卵巢抑制组5年无疾病生存率为86.6%,单独他莫昔芬组为84.7%(疾病复发,二次浸润性癌或死亡的HR=0.83;CI 0.66~1.04,P=0.10)。对治疗后影响因素分析结果显示,他莫昔芬辅助卵巢功能抑制治疗效果优于单独使用他莫昔芬治疗(HR=0.78, 95% CI 0.62~0.98)。大部分复发患者为治疗前接受过化疗的患者,在他莫昔芬辅助卵巢功能抑制组中,5年未发生复发的比例为82.5%,在他莫昔芬单独治疗组中,该比例为78.0%(HR=0.78, 95% CI 0.62~1.02)。依西美坦辅助卵巢功能抑制组的5年未发生复发比例为85.7% (与单独使用他莫昔芬组相比HR=0.65, 95% CI 0.49~0.87)
在整个研究人群中,他莫昔芬辅助卵巢功能抑制治疗并没有明显的益处。然而,对于那些有高风险复发并需要术后辅助化疗的女性,以及仍处于绝经前的卵巢癌患者,辅助卵巢抑制治疗将改善其预后。依西美坦辅助卵巢功能抑制被认为是更加完善的方案。
原始出处
Prudence A. Francis, M.D., Meredith M. Regan, Sc.D.Adjuvant Ovarian Suppression in Premenopausal Breast Cancer.NEJM.2014
本文是MedSci原创,转载请注明出处,非常感谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#绝经前#
82
#患者预后#
63
#绝经#
72
#乳腺癌患者#
55