Cell Death Dis:结直肠癌转移的新机制
2021-12-16 MedSci原创 MedSci原创 发表于上海
结直肠癌(CRC)是第三大最常被诊断为恶性肿瘤的疾病,在全球癌症死亡率中排名第三。肿瘤转移是CRC终末期患者死亡的主要原因。大多数转移性CRC患者的中位生存时间仅2年,该结果远远不能令人满意。 最近的
结直肠癌(CRC)是第三大最常被诊断为恶性肿瘤的疾病,在全球癌症死亡率中排名第三。肿瘤转移是CRC终末期患者死亡的主要原因。大多数转移性CRC患者的中位生存时间仅2年,该结果远远不能令人满意。 最近的研究发现,肿瘤微环境(TME)是一个动态的不断变化的网络,其与肿瘤细胞之间的相互作用对肿瘤的转移至关重要。CAF(癌症相关成纤维细胞)是癌细胞周围基质细胞的主要成分之一,其和CRC细胞之间的代谢性相互作用在CRC的发生发展过程中起着重要作用。然而,关于CAF的脂质改变以及这些代谢重编程是如何影响CRC细胞的转移目前还不明确。
在该研究中,研究人员发现与正常成纤维细胞的条件培养基(CM)相比,CAFs的条件培养基能够促进CRC细胞的迁移。CAF受到脂质组重编程作用并积累了更多的脂肪酸和磷脂。研究发现去除了蛋白质的CAFs条件培养基仍然能够促进CRC细胞的迁移,这表明CAFs条件培养基中的小分子代谢产物是提高CRC细胞迁移的原因。
研究人员进一步明确CRC细胞吸收了CAF细胞分泌的脂质代谢产物。FASN(脂肪酸合酶)是脂肪酸合成的关键酶,在CAF中其表达水平显著升高。通过siRNA敲低FASN的表达或者通过使用外源磺基N-琥珀酰亚胺基油酸钠或内源CD36单克隆抗体减少CRC细胞对脂肪酸的摄取,可以有效的抑制CAF诱导的CRC细胞迁移作用。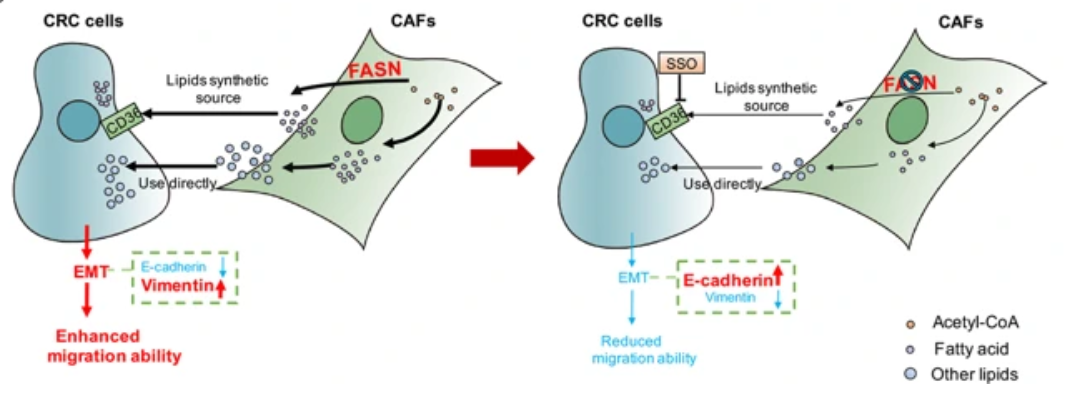
总而言之,该研究结果阐述了一个新的结直肠癌的转移机制,提示癌症相关成纤维细胞中的FASN基因和结直肠癌细胞中的CD36基因可能是癌症抗转移治疗的潜在靶标。
原始出处:
Gong et al. Reprogramming of lipid metabolism in cancerassociated fibroblasts potentiates migration of colorectal cancer cells. Cell Death and Disease (2020) 11:267
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
81
#CEL#
54
#Dis#
66
#结直肠#
69
#Death#
108
#癌转移#
118