J Clin Periodontol:低剂量阿司匹林对牙周病的治疗并无影响
2015-04-11 MedSci译 MedSci原创
J Clin Periodontol:低剂量阿司匹林对牙周病的治疗并无影响关键词:全国健康和营养调查研究 牙周疾病 牙周炎 阿司匹林 宿主调节治疗 流行病学来自美国明达苏大学的一项研究表明,低剂量的阿司匹林与牙周炎的治疗并无关系,此研究结果这与已有的研究结论相反,该研究相关文献于2015年2月12日在线发表于 JOURNAL OF CLINICAL PERIODONTOLOGY《临床牙周

来自美国明达苏大学的一项研究表明,低剂量的阿司匹林与牙周炎的治疗并无关系,此研究结果这与已有的研究结论相反,该研究相关文献于2015年2月12日在线发表于 JOURNAL OF CLINICAL PERIODONTOLOGY《临床牙周病杂志》。
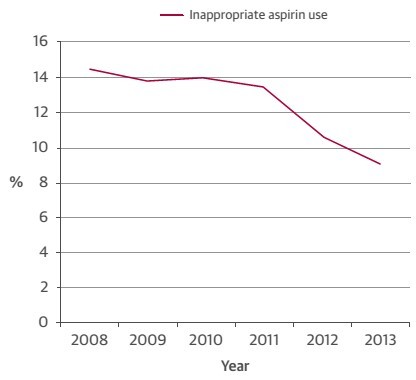
以往的研究表明低剂量的阿司匹林可作为宿主调节剂辅助治疗牙周炎。该研究调查了地基梁阿司匹林与牙周炎患病率之间的关系。
研究纳入了2335例成年男性和女性,平均年龄(SE)为55.8岁(0.42)所有研究对象均接受全口牙周检查,并填写关于阿司匹林使用的问卷。牙周检查包括全口平均探诊深度,附着丧失程度,同时记录牙齿丧失的数目。将阿司匹林使用≤162g/天定义为低剂量。
检查结果显示49.5%的研究对象为牙周炎患者,25%的研究对象使用了低剂量的阿司匹林。多因素 logistic回归模型控制了年龄、性别、种族、社会经济状况以及其他疾病,使用低剂量阿司匹林的中度牙周炎患者的比值比(95%CI为0.56-1.50)为0.91,使用低剂量阿司匹林的重度牙周炎患者的比值比(95%CI为0.74,1.50)为1.06。
该横断面研究具有局限性,从该研究结果来看,在美国具有代表性的成年人样品中,低剂量的阿司匹林与牙周病的患病率并无关系。该研究的实践意义在于,该研究结果与先前的研究结果冲突,因此需要更多的研究来探究低剂量阿司匹林在牙周炎治疗中所起到的作用,从而更好的了解哪些牙周炎患者可从低剂量阿司匹林的使用中受益。
原始出处:
Kotsakis GA, Thai A, Ioannou A, Demmer RT, Michalowicz BS.Association between Low-dose Aspirin and Periodontal Disease: Results from The Continuous National Health and Nutrition Examination Survey (NHANES) 2011-2012.J Clin Periodontol. 2015 Feb 12. doi: 10.1111/jcpe.12380.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











好文章,还会关注
97
#低剂量阿司匹林#
76
#PE#
59
临床上默认有用
106
#牙周病#
82
#牙周#
0
#低剂量#
72
有用
166