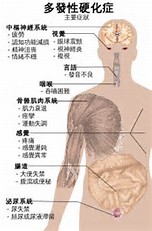
JAMA Neurol:多发性硬化的视网膜结构、鞘内免疫与临床病程的关系
2017-05-05 zhangfan MedSci原创
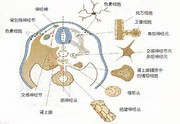
视网膜层可以反映多发性硬化病情的进展。GCIPL减少与鞘内B免疫细胞增加相关,是残疾恶化的独立危险因素,而INL水平与脑实质性活动有关。因此,视网膜光学相干断层扫描可能是一种对不同MS患者进行鉴别开展个体化治疗方案的手段
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#临床病程#
81
#Neurol#
58
#多发性#
66
#视网膜#
66
学习一下谢谢分享
78