AJRCCM:肺动脉高压不同人群的存活率
2021-11-01 刘少飞 MedSci原创
关于肺动脉高压 (PAH) 疾病表现和结果的种族/民族差异的可用信息有限。尽管对欧洲血统样本中遗传变异的影响进行了全面调查,但种族/民族对第1组PAH的死亡率、功能状态和疾病严重程度的影响尚不可知。

肺动脉高压 (PAH) 是一种罕见的疾病,其特征是肺血管系统的病理性闭塞性重塑,导致肺血管阻力 (PVR) 增加、右心衰竭和死亡。尽管患病率较低,但世界肺动脉高压研讨会 (WSPH) 第 1 组 PAH 疾病被认为是致命的,未经治疗的 5 年生存率为 40% 至 60%。PAH 的遗传研究还表明,与罕见变异或常见遗传变异携带者存在不同的生存关联。少数研究的初步观察表明,非裔美国人(AA)患者的潜在疾病严重程度和死亡率更高。然而,最近的一项研究未能显示出类似的趋势。还描述了治疗反应的种族差异,观察到 AA 患者的获益减少。尚不清楚这些基于种族/民族的 PAH 的初步观察是否反映了病理生理学差异;不同的疾病表型;遗传差异;或种族在环境、社会经济地位和获得护理方面的差异。
尽管 AA 人口有相互矛盾的数据,但对美国最大的少数族裔西班牙裔人口知之甚少。西班牙裔患者通常在国家登记处下落不明或代表性不足,这对研究该人群的疾病易感性和严重程度提出了重大挑战。尽管对欧洲血统样本中遗传变异的影响进行了多项调查,但此类调查不适用于混合或非欧洲人的 PAH 患者。
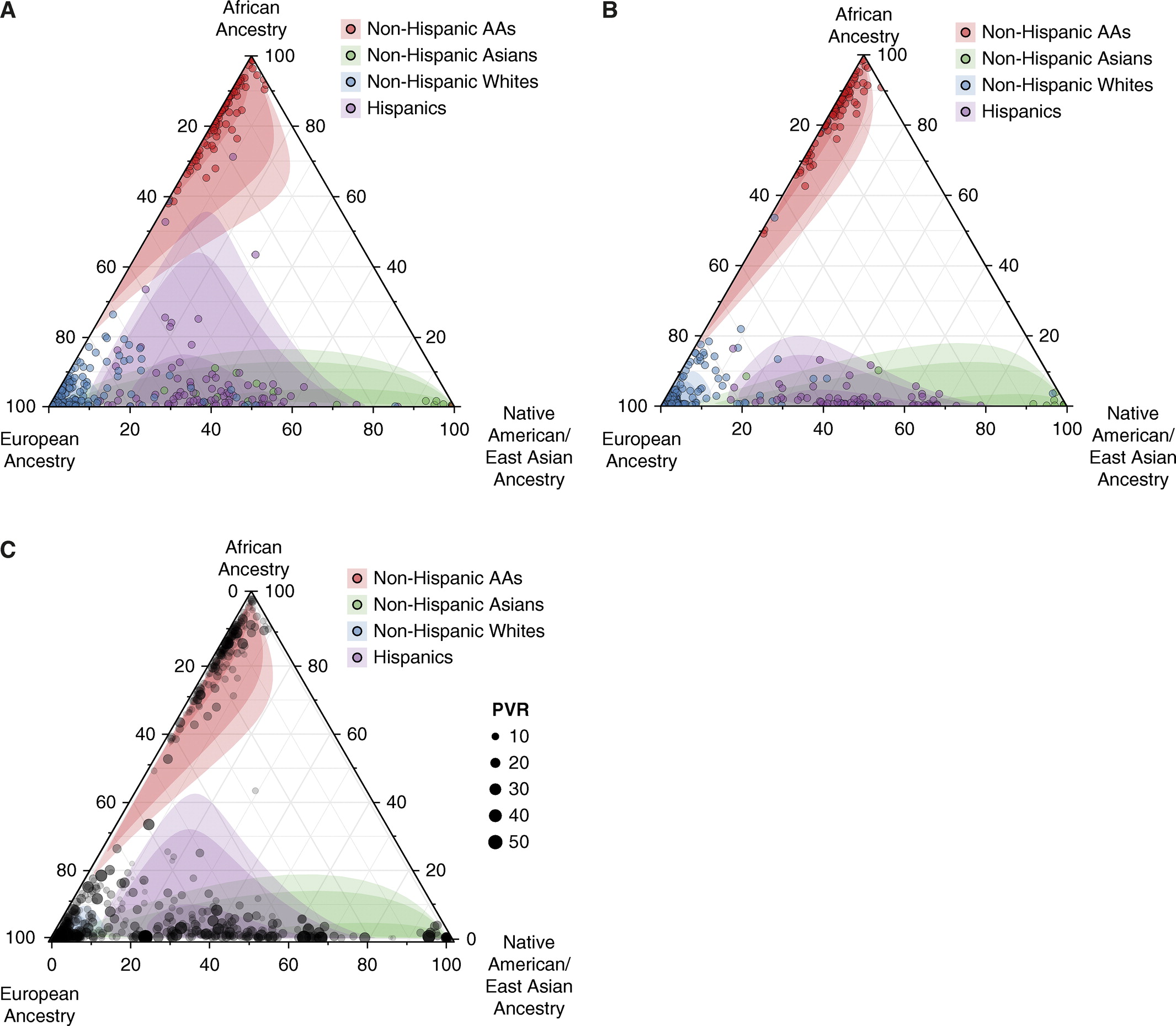
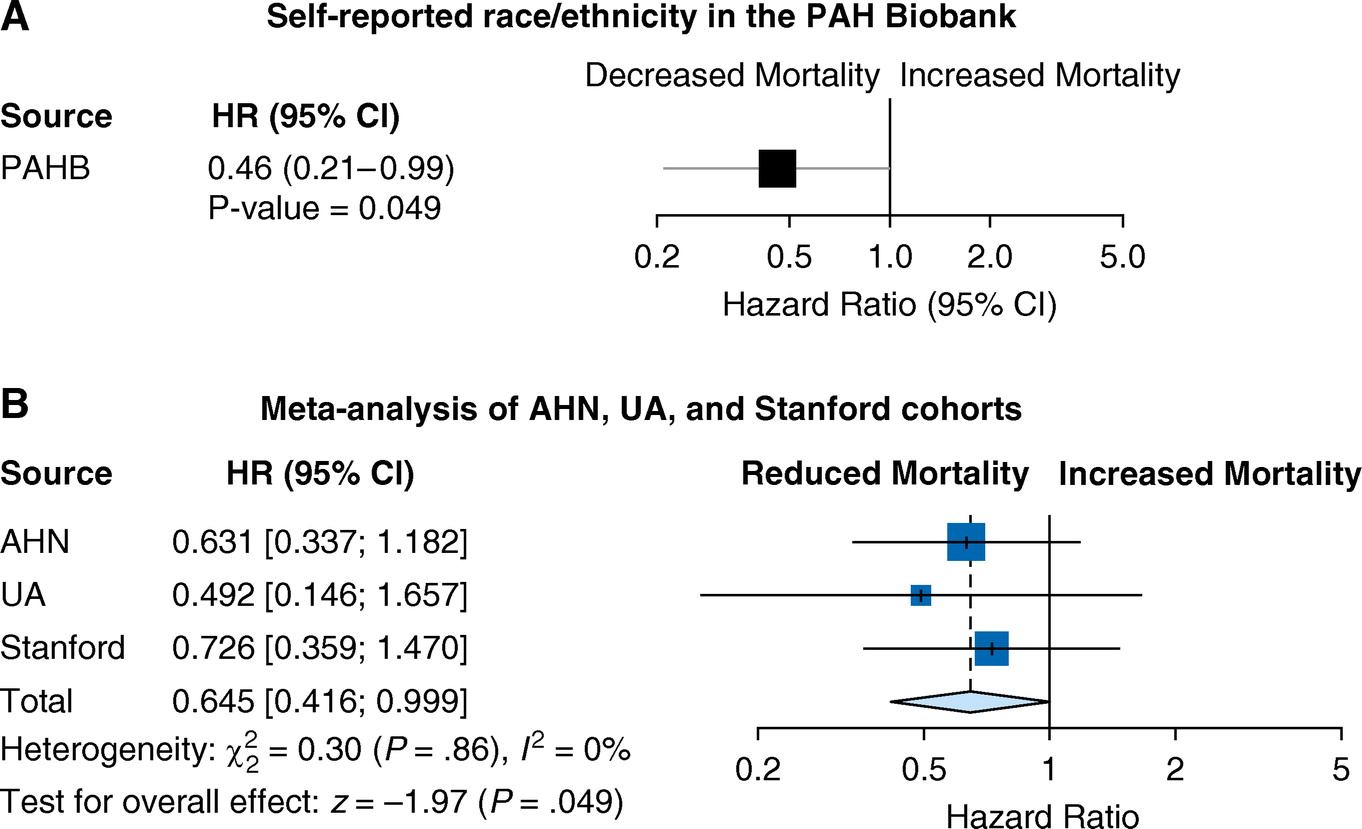
基于个别机构登记处少数族裔代表的小样本量,本研究确定了种族/民族和全球遗传血统对来自全国样本的特发性或可遗传 (I/H) PAH 病例相对同质人群的死亡率和功能状态的影响PAH。然后,研究对所有第 1 组 PAH 病例进行了这些分析,结合了三个额外的独立队列,包括另一个较小的国家样本库(阿勒格尼健康网络 [AHN] 队列)和两个西班牙裔丰富的机构登记处(亚利桑那大学 [UA] 队列和斯坦福大学队列)。接下来,该研究对 PAH 的所有四个队列进行了联合分析,并评估了种族/民族对来自国家住院样本 (NIS) 数据库的特发性 PAH (IPAH) 病例住院死亡率的影响。
研究队列:
从 PAH 生物库 (n = 1,326)、AHN 队列 (n = 822)、UA 队列 (n = 164) 和斯坦福队列 (n = 203) 中共确定了 2,515 例第 1 组 PAH 病例。 该总数包括 1,970 名 NHW 患者、255 名 AA 患者和 290 名西班牙裔患者。
种族/民族对 PAH 登记处死亡率的影响:
尽管个别队列缺乏足够数量的少数族裔受试者进行生存分析,但我们在来自 PAH 生物库的 I/H PAH 患者的同质队列中观察到,报告的西班牙裔种族可显着降低死亡率(风险比 [HR],0.46 [0.21 –0.99];P = 0.049)
NIS 数据库中种族/民族对死亡率的影响:
在未纳入荟萃分析的 NIS 数据库中,确定了 8,829 名 NHW、2,628 名 AA、1,524 名西班牙裔、403 名亚洲人和 185 名美洲原住民患有第 1 组 PAH。在 NIS 数据库中,西班牙裔患者在住院期间与 NHW 患者相比显示出显着的死亡率获益(优势比 [OR],0.65 [0.50–0.84];P = 0.001)。
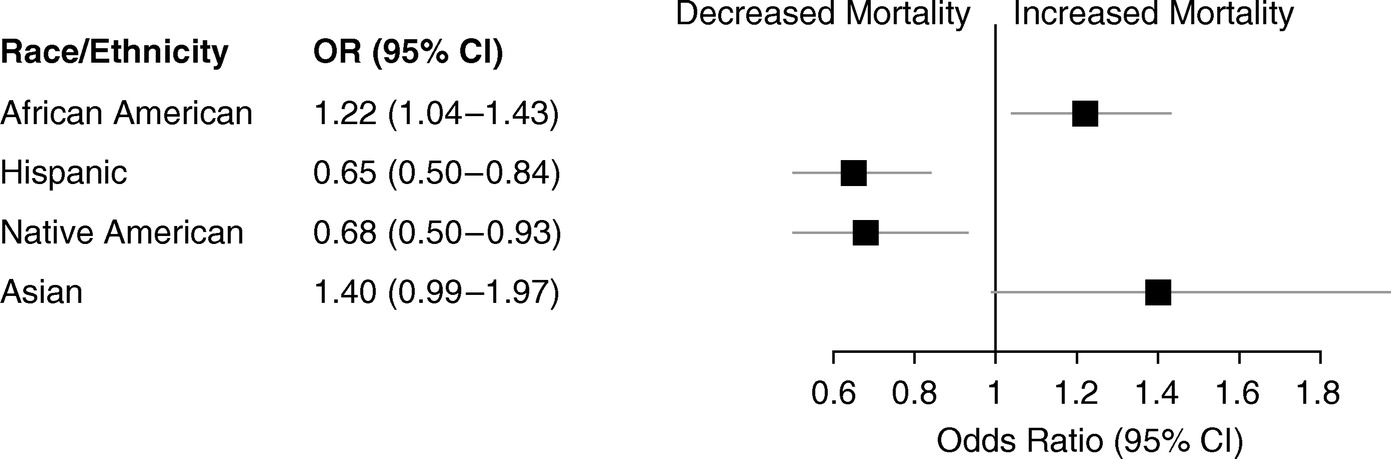
这项研究报告了对第 1 组 PAH 中种族、民族和混合的综合评估,这通过具有全基因组数据的 PAH 患者的国家资料库成为可能。详细介绍了自我报告的种族/民族、基因定义的种族/民族和血统对五个队列中西班牙裔和非裔美国人人群全因死亡率的影响。该研究表明,在多种临床环境中,第 1 组 PAH 的西班牙裔患者具有可重复的生存获益。结果表明,对西班牙裔患者生存率提高的观察强调需要进行强有力的研究来评估血统和混合对临床结果的影响。结果强化了 PAH 中种族/族裔差异的存在,表明这些差异部分是由于种族/族裔群体之间的遗传差异。
研究出处:
Karnes JH, Wiener HW, Schwantes-An TH, Natarajan B, Sweatt AJ, Chaturvedi A, Arora A, Batai K, Nair V, Steiner HE, Giles JB, Yu J, Hosseini M, Pauciulo MW, Lutz KA, Coleman AW, Feldman J, Vanderpool R, Tang H, Garcia JGN, Yuan JX, Kittles R, de Jesus Perez V, Zamanian RT, Rischard F, Tiwari HK, Nichols WC, Benza RL, Desai AA. Genetic Admixture and Survival in Diverse Populations with Pulmonary Arterial Hypertension. Am J Respir Crit Care Med. 2020 Jun 1;201(11):1407-1415. doi: 10.1164/rccm.201907-1447OC. PMID: 31916850; PMCID: PMC7258627.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉高压#
92
#RCC#
108
#存活率#
119
学习了
83
学习
107
涨知识,努力学习
122