European Radiology:哪些乳腺癌患者需要进行化疗后的MRI检查?
2023-11-25 shaosai MedSci原创 发表于上海
据报道,MRI预测浸润性乳腺癌对NAC的病理完全反应(pCR)的能力在52%和74%之间。因此,目前的政策建议在NAC之后进行手术取样以明确诊断。
现阶段,新辅助化疗(NAC)是局部晚期乳腺癌(LABC)患者的一种成熟的治疗选择。新辅助化疗的主要优点是能够消除或减少一些最初被评估为无法切除或需要切除的肿瘤,从而使新辅助化疗后能够选择保乳手术(BCS)。其他优势还包括对治疗反应的体内监测、对预后的预测,以及减少对腋窝切除的需求。
NAC术后详细而精确的影像学检查对于确定残余疾病的存在和程度以及指导进一步治疗至关重要。虽然体格检查、乳腺钼靶检查和超声波的诊断精度有限,但MRI已被确定为最准确的成像方式,目前被美国放射学会和欧洲乳腺成像协会推荐用于评估NAC的反应。MRI既能量化残余肿瘤的数量,又能描绘出反应的模式,从而确定乳腺内残余肿瘤的范围,为NAC后的手术计划提供关键信息。乳腺MRI在描述残余疾病方面具有较高的敏感性和PPV,分别为86%和93%。据报道,MRI预测浸润性乳腺癌对NAC的病理完全反应(pCR)的能力在52%和74%之间。因此,目前的政策建议在NAC之后进行手术取样以明确诊断。虽然不同等级的肿瘤和分子亚型的MRI预测pCR的准确性不同,但据我们所知,到目前为止还没有研究对钙化乳腺癌与非钙化乳腺癌的肿瘤反应预测进行评估。
近日,发表在European Radiology杂志的一项研究探讨了NAC后MRI增强是否可以为乳腺钙化患者手术范围的提供更加准确的信息。
本项研究于2011年至2018年对114名NAC患者进行了回顾性分析,包括人口统计学、乳腺钼靶检查、3个T-MRI和病理学,比较了两个亚组:没有(n = 62)或有(n = 52)乳腺钼靶检查显示的钙化。在钙化队列中,乳腺钼靶检查的钙化程度和MRI的增强程度是重叠的。MRI预测对NAC的反应与病理学相关。采用双尾配对T检验和Fisher's精确检验以及Cohen's kappa系数进行了分析。
两个亚组在人口统计学方面没有明显差异。肿瘤的大小、淋巴结受累和DCIS成分方面表现出同等特征。ER阴性/HER2阳性肿瘤更常出现钙化(33% n = 17钙化vs 13% n = 8非钙化;p < 0.05);三阴性病理很少出现钙化(6% n = 3钙化vs 33% n = 20非钙化;p < 0.05)。NME更常见钙化(62% n = 32钙化vs 29% n = 18非钙化;p < 0.05)和无钙化的增强(90% n = 56非钙化vs 81% n = 42钙化;p < 0.05)。两组对NAC的反应相似(pCR=37%非钙化vs 38%钙化);MRI上的反应与病理同样相关(两个亚组都是69%;p=0.988)。
图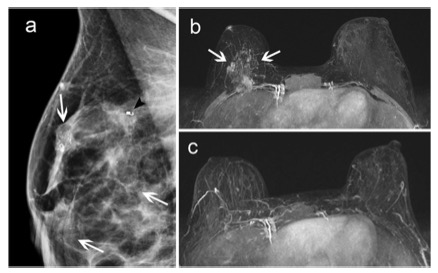
26岁患者,患有IDC 3级ER阴性PR阴性HER2阳性乳腺癌。治疗前MLO乳腺图(a)显示右测乳腺广泛的钙化(白色箭头)和活检后的夹子(黑色箭头)治疗前MRI T1W减去MIP图像(b)显示与乳腺图钙化相关的广泛增强(箭头)。治疗后的MRI(c)显示增强的影像学表现完全消失。患者接受了右乳切除术以确保完全切除钙化。在手术病理中,确定了完全的病理反应,从而建立了MRI预测和手术病理结果之间的良好相关性
本项研究结果显示,建议在计划手术时利用NAC后的MRI结果进行评估而不是乳腺钼靶检查,因为MRI的预测独立于钙化的存在与否。同时,有必要进行前瞻性研究来评估这种方法的临床意义及价值。
原文出处:
Tamar Sella,Bar Simor,Yael Adler-Levy,et al.MRI prediction of neoadjuvant chemotherapy response is equivalent in patients with or without mammographic calcifications: a step towards adapting surgical approach?DOI:10.1007/s00330-023-09640-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习学习
100
学习了,谢谢分享
84
好文章,谢谢′分享。
78
不错,学习了。
73
#乳腺癌# #新辅助化疗#
100