当你的手不再属于你,它开始自主行动的时候......
2017-12-20 MedSci MedSci原创
今天的标题看起来是幻想中的故事,令人不可置信,然而这是确确实实的一种疾病。该病由于大脑内侧前区的运动神经受损造成的,通常在大脑手术、中风 或大脑感染之后,很容易出现。

今天的标题看起来是幻想中的故事,令人不可置信,然而这是确确实实的一种疾病。该病由于大脑内侧前区的运动神经受损造成的,通常在大脑手术、中风 或大脑感染之后,很容易出现。
病史:
患者为一42岁中年女性,既往有糖尿病病史6年;高血压病病史5年,血压最高达180/120mmHg,糖尿病与高血压均未经系统治疗,未定期检测血糖及血压。
患者自述入院前半月无明显诱因出现左侧肢体活动不灵,以左上肢为著,主要表现为左手不受自己控制,与右手唱反调,如右手扣纽扣,左手接着就把纽扣解开或右手提上裤子,左手就脱下裤子等,同时伴有言语笨拙,但能理解他人言语,上述症状呈持续性。
查体:
患者神志清,精神一般,意识清楚,构音障碍,双眼各向运动自如,双侧瞳孔等大同圆,双眼对光反射灵敏,双侧额纹等深对称,鼻唇沟等深对称,伸舌居中,咽反射正常,双肺呼吸音清,未闻及干湿性啰音,心音低钝,律齐,各瓣膜听诊区未闻及杂音。腹部平软,未见异常。双下肢无水肿。左上肢肌力4级,四肢肌张力正常,四肢腱反射对称引出,双侧病理征未引出,感觉系统未查及异常,双侧指鼻试验稳准,跟膝胫试验未见异常,余神经系统查体未见异常。
辅助检查:
颈部血管彩超:颈动脉硬化伴斑块形成,右侧椎动脉起始部狭窄。
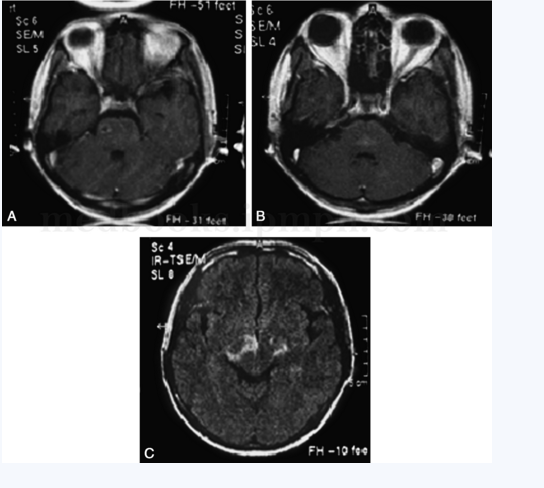
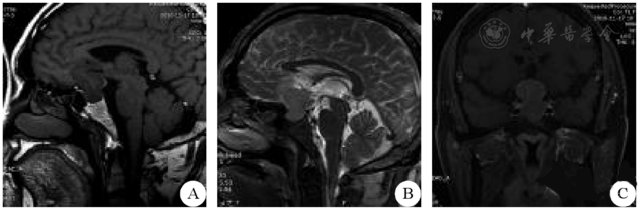
头部MRI平扫:右侧胼胝体膝部、体部、压部可见斑片状长T1、长T2信号影,边界欠清,Flair呈稍高信号。
头部DWI:右侧胼胝体膝部、体部、压部可见斑片状稍高信号,边界不清。
头部MRA:Willis环完整,双侧大脑中动脉M1段、双侧大脑后动脉P1段、双侧椎动脉末端、基底动脉、双侧大脑前动脉管壁凹凸不平,局部显示不清;右侧颈内动脉末端局限性中-重度狭窄。
血糖检测:急诊静脉血糖GLU14.1mmol/L、空腹静脉血糖GLU16.24mmol/L、糖化血红蛋白10.40%
大生化:甘油三酯TG2.44mmol/L、低密度脂蛋白胆固醇LDLC2.99mmol/L、血尿素氮6.1mmol/L、血清肌酐86μmol/L、谷丙转氨酶22U/L、谷草转氨酶18U/L
血常规:白细胞计数5.0×10^9/L、红细胞计数4.6×10^12/L、血红蛋白浓度148g/L、血小板计数160×10^9/L
简要解析:
本病主要表现为一侧上肢或手不自主的、不能控制的和无目的的运动,伴有患者对自己受累的肢体的陌生感和拟人格化。临床表现将本病分为5种主要亚型:
(1)对抗失用或手间冲突:表现为当指令健侧手执行某一项动作时,患侧手则出现与执行动作完全相反的对抗和干扰行为,主要发生在非优势手。该患者属于此型;
(2)竞争性失用:表现为当要求患者用某只手完成指令时,患者仅用健侧手抢先完成,并自述无法控制健侧手的行为,两手均可发生;
(3)反常手或任性手:表现为患侧手反复出现冲动性活动或无法自控的行为,健侧手则对其活动加以限制,主要发生在病灶对侧手;
(4)异己手感觉:AHS的最早的概念,患者主观感觉患侧手不属于自己,伴患侧手的不自主运动,主要发生在非优势手;
(5)多余手:表现为患者自感3只或更多的手,且多余的手多为左手。
本病按病变部位分可分为额叶型、胼胝体型和后部型。
本例患者为右利手,主要表现为手间冲突,表现为当指令右侧手执行某一项动作时,左侧手则出现与执行动作完全相反的对抗和干扰行为。该患者属于胼胝体型。头部DWI示右侧胼胝体膝部、体部、压部梗死。胼胝体嘴、膝、体部由大脑前动脉供血,压部由大脑后动脉供血。因为大脑前、后动脉之间存在很多吻合支,所以较少出现胼胝体的血管病变。本例患者头部MRA示颅内多发性动脉粥样硬化特别是后循环多发性狭窄,提示该患者大脑前、后动脉对胼胝体区的供血都存在不足,从而出现胼胝体梗死。而造成该患颅内多发性动脉粥样硬化的主要原因可能是该患长期的高血压、糖尿病及吸烟、酗酒病史等。
完整病例请前往【梅斯医生】→病例库→神经科→“左侧肢体活动不灵伴言语笨拙半月”
更多点评分析,趣味的学习,详情尽在梅斯医生上,您可以在这里体验模拟诊疗。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了谢谢分享
145
学习了.涨知识
101
学习学习学习
129
不错不错.学习了
99
谢谢分享学习了
105