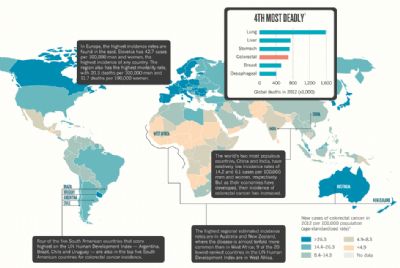
Nature专题:第四大致命癌症大肠癌
2015-05-18 佚名 生物通
每年夺走近70万人的生命,大肠癌(Colorectal cancer,CRC)成为了仅次于肺癌、肺癌和胃癌的全球第四大最致命的癌症。大肠癌是一种现代疾病:在发达国家具有最高的发病率。但随着全球变得更为富有,越来越多的人转向西方饮食和生活方式,大肠癌的发病率还有可能增加。 最新一期(5月14日)的Nature杂志以“Outlook: Colorectal cancer
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











这篇文章有一定深度
136
是一篇不错的文章
90
#Nat#
62
#专题#
66
非常有用!很全面!
117
你以为找治愈方法那么容易哇!
117
额
118
赶紧找到治愈方法!
106
可怕!
186