Cell Reports:用维生素D治疗糖尿病
2015-03-23 叶予 生物通
二型糖尿病和心脏病常常同时发生,近年来人们发现这两种疾病与维生素D缺乏有关。 慢性炎症会引起胰岛素抵抗和堵塞动脉的斑块,是二型糖尿病和心脏病的根源。华盛顿大学的科学家们发现维生素D能够防止这样的炎症,而且维生素D不足会影响一种关键的免疫细胞。这项研究发表在三月十九日的Cell Reports杂志上。 研究显示,免疫细胞缺乏维生素D受体,会使小鼠抵抗胰岛素的作用,导致体内的葡萄糖过量。
二型糖尿病和心脏病常常同时发生,近年来人们发现这两种疾病与维生素D缺乏有关。
慢性炎症会引起胰岛素抵抗和堵塞动脉的斑块,是二型糖尿病和心脏病的根源。华盛顿大学的科学家们发现维生素D能够防止这样的炎症,而且维生素D不足会影响一种关键的免疫细胞。这项研究发表在三月十九日的Cell Reports杂志上。 [pdf free]
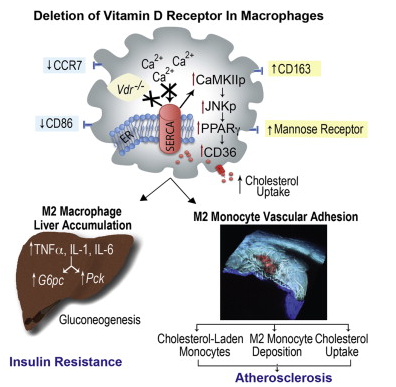
研究显示,免疫细胞缺乏维生素D受体,会使小鼠抵抗胰岛素的作用,导致体内的葡萄糖过量。此外,小鼠血管中也会出现斑块累积。
“我们发现维生素D有助于调控葡萄糖代谢,这可以解释为何缺乏维生素D的人更容易患糖尿病,”文章的资深作者,华盛顿大学的副教授Carlos Bernal-Mizrachi说。“在我们的研究中,失活维生素D受体会引起糖尿病和动脉粥样硬化。反过来,恢复维生素D的水平应该可以起到治疗效果。”
研究人员还发现,维生素D不足会使单核细胞成为脂肪转运者。单核细胞是免疫系统中的一种白细胞。它们从骨髓进入血液的几天后,往往会移动到组织中,在那里成熟为巨噬细胞。
“失活单核细胞和巨噬细胞上的维生素D受体,会增强肝脏和动脉壁的炎症,” Bernal-Mizrachi说。“单核细胞附着到血管壁的能力也会提高,在那里释放出与糖尿病和心脏病有关的胆固醇和炎症性物质。” 补充足够的维生素D,也许能减少这些问题,避免心脏病和糖尿病的并发。
这是人们首次发现,缺乏维生素D的单核细胞会把脂肪带到血管壁。“我们知道,单核细胞成熟为巨噬细胞之后就能摄取胆固醇,”文章的共同第一作者,助理教授Amy E. Riek说。“但我们在实验中发现,在缺乏维生素D时,血液里的单核细胞也能吃掉并携带胆固醇。”
这一发现很重要,因为靶标血液中的物质比靶标血管壁中的物质容易得多。这项研究“为我们提供了潜在的治疗靶标,”Riek说。
研究人员将正常骨髓移植到出现了二型糖尿病和动脉粥样硬化的缺陷型小鼠中,成功降低了这些小鼠体内的炎症和血糖水平,让小鼠对胰岛素更加敏感。现在他们正在临床试验中用维生素D治疗二型糖尿病患者,希望能够避免一些并发症。
原始出处:
Jisu Oh, Amy E. Riek, Isra Darwech,et,al.Deletion of Macrophage Vitamin D Receptor Promotes Insulin Resistance and Monocyte Cholesterol Transport to Accelerate Atherosclerosis in Mice .Cell Reports.doi:10.1016/j.celrep.2015.02.043[pdf free]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cell#
71
#CEL#
69
好好学习一下
166
AKI对心衰临床治疗意义重大,但依然需要研究检验其适用性
161
学习啦
149
学习啦
166
学习啦
122
这仅仅是基础研究,与临床不同
168