Heart:导管消融和抗心律失常药物治疗后房颤复发的性别差异
2022-03-26 MedSci原创 MedSci原创
虽然心房颤动导管消融后女性的心律结局比男性患者差,但老年女性的抗心律失常药物后反应优于男性。
性别差异正在成为各种心血管疾病的一个重要问题。心房颤动在韩国人群中的患病率已达到 1.6%,并且还在不断增加。心房颤动的发病率在男性中明显较高,但女性患心房颤动的比例随着年龄的增长而增加。此外,女性心房颤动导管消融后复发的风险高于男性。然而,目前尚不清楚复发患者的抗心律失常药物反应性是否存在性别差异。

近日,心脏病领域权威杂志Heart上发表了一篇研究文章,在2999例接受新生心房颤动导管消融的患者(26.5% 为女性,平均年龄为58.3±10.9岁,68.1%为阵发性心房颤动患者)中,研究人员比较和评估了1094例复发患者和788例随后接受抗心律失常药物进行节律控制患者节律结局的性别差异。
在48.2±34.9个月的随访中,1094例患者(36.5%)在接受心房颤动导管消融术后发生心房颤动复发,788例接受抗心律失常药物的患者中有508例(64.5%)发生心房颤动复发。
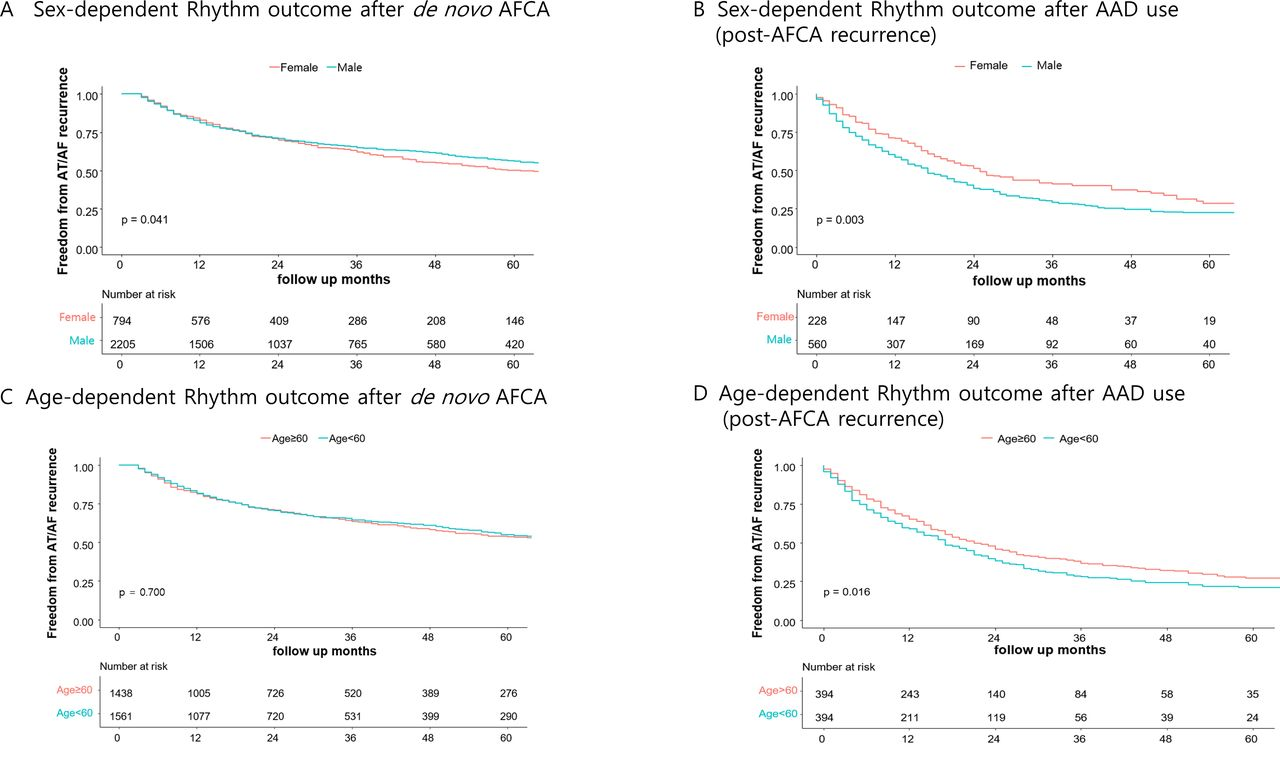
虽然心房颤动导管消融的节律结局在女性中更差(对数秩p=0.041,HR为1.28,95%CI为1.02至1.59,p=0.031),但女性术后复发后的抗心律失常药物反应优于男性(对数秩p=0.003,HR为0.75,95%CI为0.59至0.95,p=0.022),尤其是在60岁以上的女性中(对数秩p=0.003)。在使用抗心律失常药物后249名患者接受了重复手术,女性的肺静脉(PV)重新连接率(62.7% vs. 76.8%,p=0.048)低于男性,但不存在额外PV触发因素(37.8% vs. 25.4%,p=0.169)。
由此可见,虽然心房颤动导管消融后女性的心律结局比男性患者差,但老年女性的抗心律失常药物后反应优于男性。
原始出处:
Yoon Jung Park.et al.Sex difference in atrial fibrillation recurrence after catheter ablation and antiarrhythmic drugs.heart.2022.https://heart.bmj.com/content/early/2022/03/23/heartjnl-2021-320601
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ART#
64
#导管消融#
93
#消融#
73
#HEART#
60
#抗心律失常药物#
64