最新一期《美国心脏病学会杂志》(JACC)发表了第二军医大学长海医院血管外科教授景在平领衔的“升主动脉夹层腔内微创治疗疗效评估”研究成果。国际血管领域权威专家、主动脉疾病腔内治疗先驱Michael D. Dake教授专门为此论文在JACC作长篇述评。这标志着我国在主动脉疾病腔内微创治疗技术领域已走在世界前列。
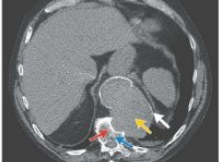
累及升主动脉的Stanford A 型主动脉夹层是最为凶险的血管系统疾病之一,以体外循环为基础的开胸大手术一直以来是升主动脉夹层的标准治疗方法。目前,虽然腔内微创技术已广泛应用于腹主动脉、降主动脉甚至主动脉弓部疾病的治疗,但一直无法有效应用于升主动脉的治疗。
景在平等率先提出指导腔内微创治疗的“主动脉3N3V新分型”,先后创用了开槽、开窗和复杂平行支架等一大批临床新技术,并成功研发了具有完全自主知识产权的主动脉弓分支型腔内移植物。该款移植物已完成全球多中心临床试验并成功转化,成为世界首款实际临床应用的主动脉弓分支型移植物。
原始出处
Michael D. Dake, MD.On the Endovascular Climb to the Type A Dissection Summit, Reaching a New Base Camp∗.JACC.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#微创治疗#
80
#JACC#
61
#微创#
61
#ACC#
51
#主动脉#
49
#动脉夹层#
76