J Gastroenterol:日本人群中Elbasvir 联合grazoprevir 治疗HCV:II/III期临床研究
2017-03-28 MedSci MedSci原创
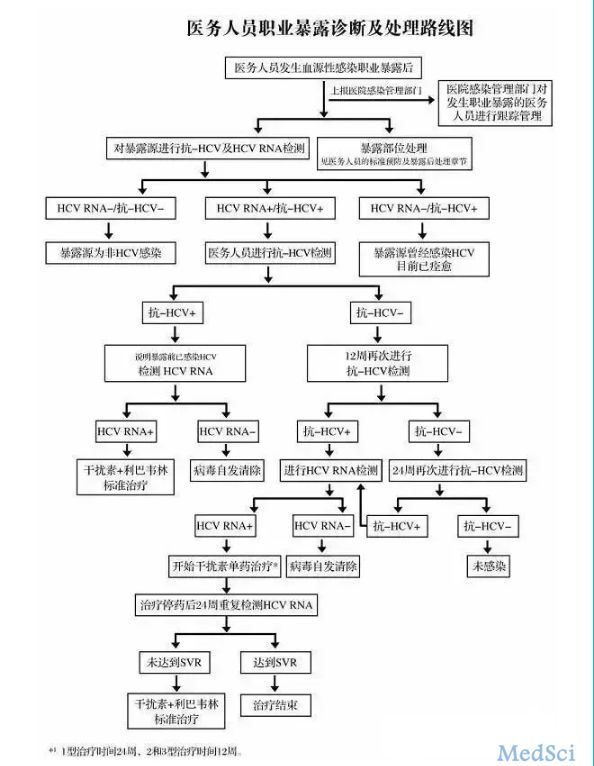
背景:Elbasvir (EBR)联合grazoprevir (GZR)治疗HCV感染业已证实有效,然而临床研究主要在美国和欧洲进行。我们旨在研究EBR和GZR在日本伴或不伴有肝脏硬化的HCV患者中的安全性和有效性。方法:研究分为两个部分。第一部分,不伴有肝硬化的患者按照1:1的比例随机接受EBR 50mg+GZR 50mg或EBR 50mg+GZR 100mg治疗12周。第二部分,不伴有肝硬化患
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#日本人#
58
#I期临床#
75
#GAS#
100
#Gastroenterol#
86
#III#
66
#III期临床研究#
47
#AST#
55
#AZ#
79
#Grazoprevir#
69
#II期临床研究#
61