DDW 2016:EMR后粘膜缺损切缘热消融可显著减少腺瘤复发
2016-06-14 佚名 中国医学论坛报
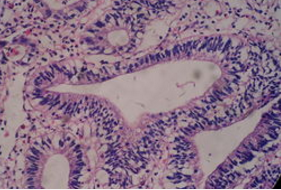
本届美国消化疾病周上,一项即将公布的研究表明,内镜下粘膜切除术(EMR)后粘膜缺损切缘行热消融可显著降低首次结肠镜监测(SC1)时腺瘤复发率,常规应用此种简单安全的技术有可能增强EMR有效性并减少监测需求。 此项前瞻性多中心研究对EMR缺损切缘行辅助热消融能否降低腺瘤复发率进行了评估。主要终点为SC1时内镜和组织学复发。将标准注射和切除EMR技术应用于所有病变。排除标准包括既往尝试治疗病变、圈套
本届美国消化疾病周上,一项即将公布的研究表明,内镜下粘膜切除术(EMR)后粘膜缺损切缘行热消融可显著降低首次结肠镜监测(SC1)时腺瘤复发率,常规应用此种简单安全的技术有可能增强EMR有效性并减少监测需求。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粘膜#
68
#热消融#
94
#EMR#
92
#消融#
89
#DDW#
77