STM:糖尿病患者骨折后愈合能力差的机制被破译
2017-01-13 佚名 生物谷
根据斯坦福大学医学院的一项最新研究,一种刺激骨干细胞活性的蛋白能够让发生骨折的糖尿病小鼠恢复得更好。研究人员在糖尿病小鼠模型和糖尿病患者的骨组织样本中观察到骨干细胞活性的下降,而这种蛋白能够抵消干细胞活性的下降。他们希望这一发现能够促进开发新方法帮助糖尿病患者从骨折中更好的恢复。相关研究结果发表在国际学术期刊Science Translational Medicine上。全世界有几亿人受到

根据斯坦福大学医学院的一项最新研究,一种刺激骨干细胞活性的蛋白能够让发生骨折的糖尿病小鼠恢复得更好。研究人员在糖尿病小鼠模型和糖尿病患者的骨组织样本中观察到骨干细胞活性的下降,而这种蛋白能够抵消干细胞活性的下降。他们希望这一发现能够促进开发新方法帮助糖尿病患者从骨折中更好的恢复。
相关研究结果发表在国际学术期刊Science Translational Medicine上。
全世界有几亿人受到糖尿病困扰,这一数字还在逐年增加。糖尿病除了会引起餐后血糖的危险波动,还会导致其他许多症状,包括软组织损伤和骨折愈合能力受损。其中的精确分子机制还没有得到充分了解。
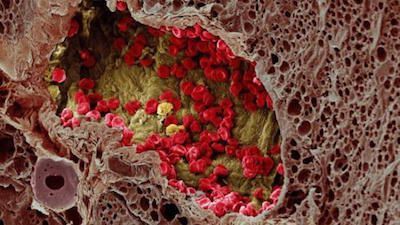
在之前的一项研究中,研究人员曾经在小鼠的骨组织中发现一群骨干细胞,这些成体干细胞可以形成骨骼系统的所有成分。去除这些成体干细胞,小鼠骨折后愈合的能力会受到严重损伤。
在这项研究中,研究人员使用了一种2型糖尿病小鼠模型,小鼠在大约4周龄开始出现糖尿病症状,但是在糖尿病发生之前,小鼠骨折愈合的效率与野生型小鼠基本没有差别。与之相比,在糖尿病发生之后小鼠的骨密度明显低于对照组,发生骨损伤后愈合能力明显变差,研究人员在骨折七天后对比了骨干细胞的数量,发现糖尿病小鼠的骨干细胞数量明显少于对照小鼠。
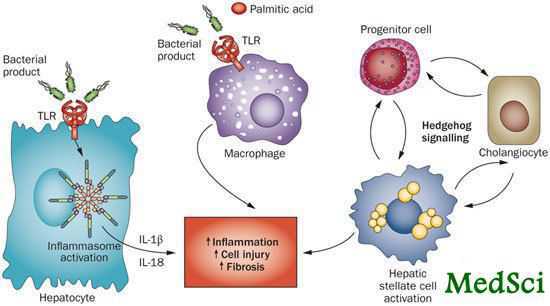
研究人员通过一系列实验排除了导致干细胞数量下降的系统原因也证实骨干细胞本身具有正常功能。随后他们对干细胞所处微环境进行了分析,发现糖尿病小鼠体内一类叫做hedgehog的信号蛋白水平明显更低,这个家族的蛋白在许多生物学过程中发挥重要作用,包括胚胎发育和组织再生。
研究人员猜测人为阻断hedgehog信号途径也能够损伤非糖尿病小鼠的骨愈合能力,而实验结果也验证了这一猜测,并且向糖尿病小鼠发生骨折的局部环境中加入hedgehog信号蛋白能够恢复小鼠的骨愈合能力。
最后研究人员又在糖尿病患者和非糖尿病患者的骨组织样本中检测了hedgehog信号途径中一些重要蛋白的表达,发现人类组织的分析结果完全符合他们在小鼠模型中观察到的现象。
这些结果表明直接靶向骨干细胞hedgehog信号途径中的一些分子可能对骨损伤后愈合有促进作用,但是在转化到临床应用之前还需要进行更多研究。

原始出处:
Tevlin R, Seo EY, Marecic O, McArdle A, Tong X, Zimdahl B, Malkovskiy A, Sinha R, Gulati G, Li X, Wearda T, Morganti R, Lopez M, Ransom RC, Duldulao CR, Rodrigues M, Nguyen A, Januszyk M, Maan Z, Paik K, Yapa KS, Rajadas J, Wan DC, Gurtner GC, Snyder M, Beachy PA, Yang F, Goodman SB, Weissman IL, Chan CK, Longaker MT.Pharmacological rescue of diabetic skeletal stem cell niches.Sci Transl Med. 2017 Jan 11;9(372). pii: eaag2809. doi: 10.1126/scitranslmed.aag2809.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#STM#
76
学习了,很好
104
原来是这样啊
95
#糖尿病患者#
63
非常好
93
然后作用呢
102
学习新知识谢谢分享。
87