JCEM:Osilodrostat治疗库欣病的随机试验
2022-04-13 从医路漫漫 MedSci原创
长期暴露于皮质醇水平升高的环境中,会导致发病率和死亡率显著增加,生活质量(QoL)受损。因此,皮质醇的正常化是库欣病的主要治疗目标。经蝶手术是大多数患者的一线治疗方法。

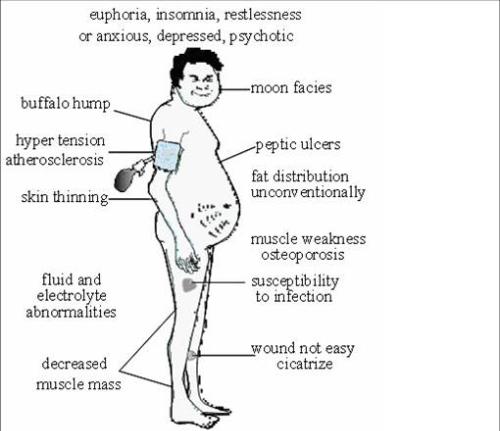
背景:库欣病是一种罕见的皮质醇增多症,由分泌促肾上腺皮质激素(ACTH)的垂体腺瘤引起,该腺瘤反过来刺激肾上腺产生过量的皮质醇。长期暴露于皮质醇水平升高的环境中,会导致发病率和死亡率显著增加,生活质量(QoL)受损。因此,皮质醇的正常化是库欣病的主要治疗目标。经蝶手术是大多数患者的一线治疗方法。然而,多达三分之一的患者在垂体手术后没有达到持续缓解,需要额外的治疗。这些患者的选择包括重复垂体手术、药物治疗、放射治疗和双侧肾上腺切除术。尽管有多种治疗选择,许多患者不能达到或维持正常的皮质醇分泌。Osilodrostat是一种强效口服11β-羟化酶(CYP11B1)抑制剂。在一项针对库欣病患者的III期研究(LINC 3)中,开放标签osilodrostat在48周内快速降低了平均尿游离皮质醇(mUFC)的排泄,并且在8周随机停药期后维持正常mUFC排泄方面优于安慰剂。
目的:与安慰剂相比,评价口服11β羟化酶抑制剂Osilodrostat对库欣病患者的安全性和有效性。设计、设置、干预和参与者:LINC 4是一项III期、多中心试验,包括一个为期12周的随机、双盲、安慰剂对照(osilodrostat:安慰剂,2:1)期,随后是一个为期36周的开放治疗期(NCT02697734)。确诊为库欣病且平均尿游离皮质醇(mUFC)排泄量≥正常(ULN)上限1.3倍的成年患者(年龄18-75岁)符合入选标准。主要结果测量:主要终点是第12周mUFC≤ULN的随机患者比例。关键的次要终点是在第36周达到mUFC≤ULN的比例(在24周的开放标签osilodrostat后)。
结果:73名患者(中位年龄39岁[范围:19-67岁];平均/中位mUFC,3.1×ULN/2.5×ULN)接受了随机的osilodrostat治疗(n=48)或安慰剂治疗(n=25)。在第12周,奥西洛前列素组(77%)比安慰剂组(8%)的患者实现了mUFC≤ULN(优势比43.4;95%可信区间7.1,343.2;P<0.0001)。反应维持在第36周,此时81% (95% CI 69.9,89.1)的所有患者达到mUFC≤ULN。安慰剂对照期间(奥西洛前列素与安慰剂相比)最常见的不良事件是食欲下降(37.5%比16.0%)、关节痛(35.4%比8.0%)和恶心(31.3%比12.0%)。
表1 LINC 4研究期间平均血清和唾液皮质醇(早晨和深夜)水平以及相对于基线的变化

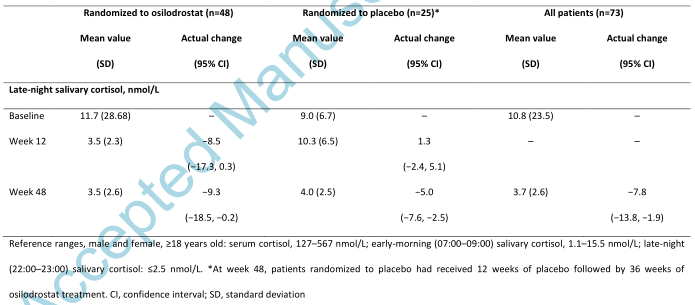
表2 LINC 4研究第48周时皮质醇增多症的身体特征相对于基线的变化
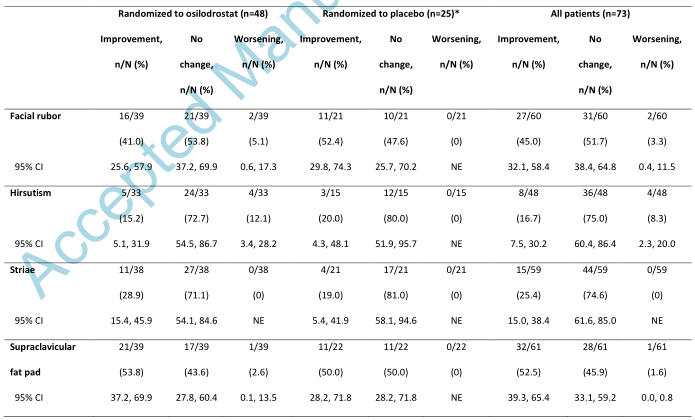
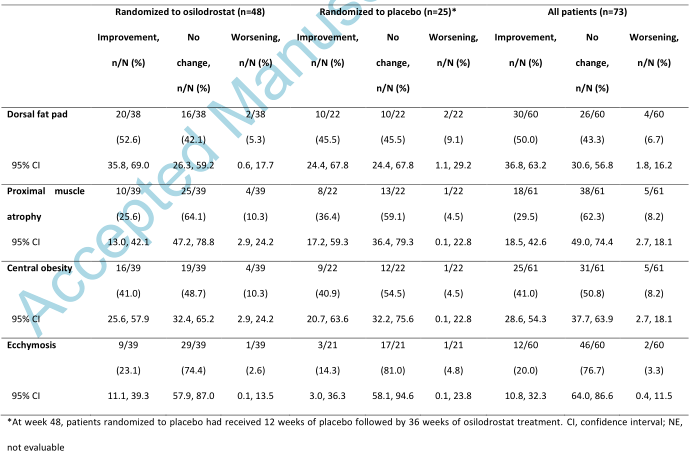
表3 第12周和第48周患者报告结果的平均变化,按随机治疗组和总体

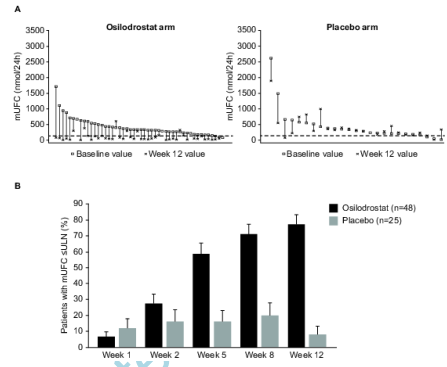
图1 (A)从基线到第12周患者体内mUFC的变化;( B)第12周mUFC ≤ULN的随机患者比例。mUFC的ULN为138 nmol/24h (50 μg/24h)。对于图A,每组垂直数据点代表一名患者,并按基线mUFC递减的顺序显示。随机分配到奥西罗司他组的6名患者和随机分配到安慰剂组的4名患者在基线时的mUFC≤1.3×ULN;然而,在筛选时,mUFC > 1.3×ULN(即患者符合资格标准)。平均尿游离皮质醇;ULN,正常值上限
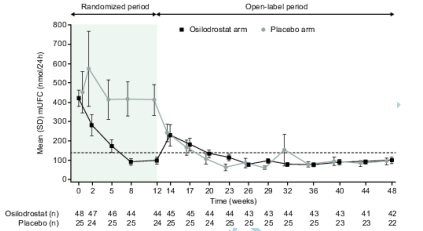
图4:随机治疗组在最高达12周和48周的时间点的平均mUFC。水平虚线表示mUFC的ULN:138 nmol/24h(50μg/24h)。平均尿游离皮质醇;SD,标准差;ULN,正常值上限
结论:在大多数库欣病患者中,Osilodrostat快速使mUFC排泄正常化,并在整个研究中保持这种效果。安全状况良好。
原文出处:Gadelha M, Bex M, Feelders RA,et al.Randomized trial of osilodrostat for the treatment of Cushing's disease.J Clin Endocrinol Metab 2022 Mar 23
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCEM#
94
#JCE#
111
#ROS#
95
#库欣病#
85
#随机试验#
75