JACC:完全性血运重建的非ST段抬高型心梗患者远期死亡率更低
2018-10-18 MedSci MedSci原创
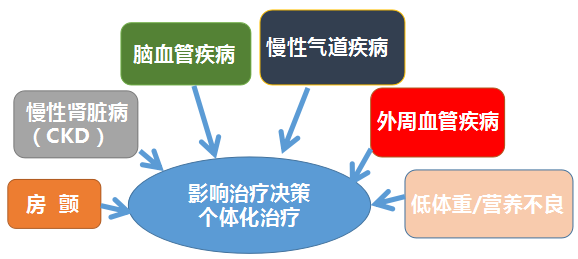
非ST段抬高型心梗(NSTEMI)患者有很大一部分会出现多血管病变(MVD),完全性的血管再生在其中起的作用尚不清楚。本研究纳入了2005-2015年伦敦的37491名NSTEMI患者,有21857名(58.3%)患者表现有多血管病变,主要终点事件的全因死亡率。经过平均4.1年时间的随访,共有11737名(53.7%)患者在PCI术中完成1期血运重建,且呈逐年增加的趋势(p=0.006)。与其他患
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#非ST段抬高#
36
#非ST段#
40
#非ST段抬高型#
45
#ST段抬高型心梗#
58
#完全性#
45
#JACC#
36
#心梗患者#
37
学习了,很不错的学习资料和临床经验,值得借鉴,获益匪浅,感谢分享!
98
#ACC#
32
#ST段抬高#
34