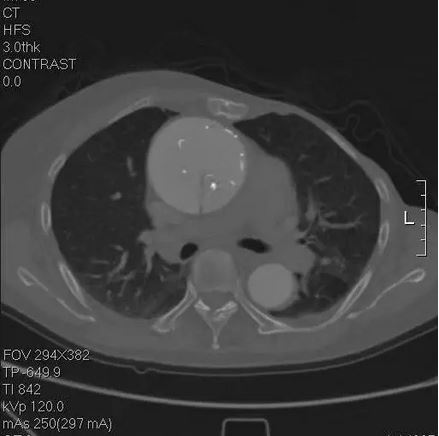
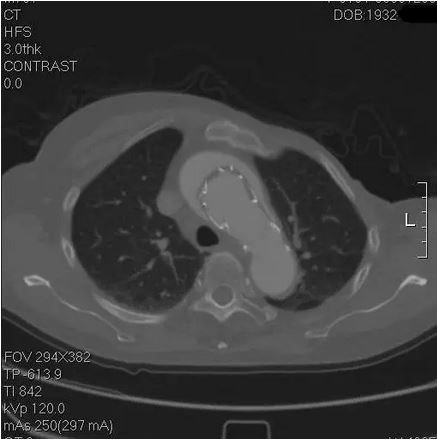
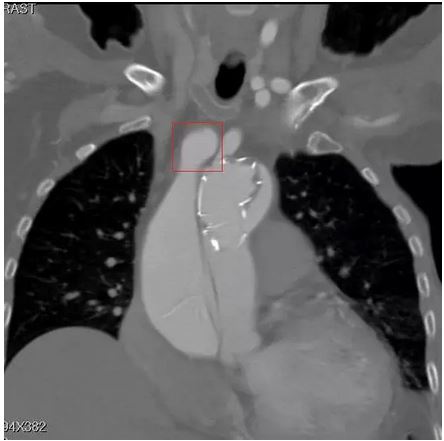
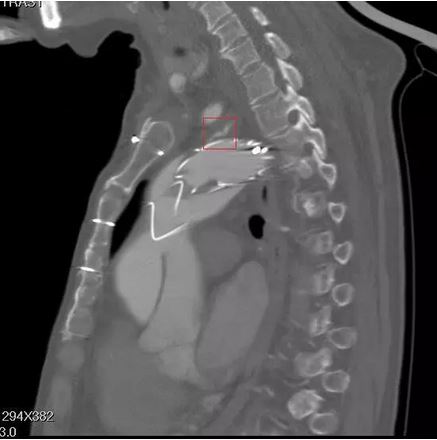
主动脉夹层袭来的恐慌,你不懂
2017-12-30 文烈心 医学界心血管频道
医学是科学,但临床医学有时没法完全遵从条规,因为医疗原则具体到某个特殊个案,可能根本不具实际可操作性。而患方,面对的恐慌无助,你也许真的不懂。




本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










说明人的适应能力很强
37
确实很奇特.不管怎么说.患者活得好好的.
43
感谢分享
45
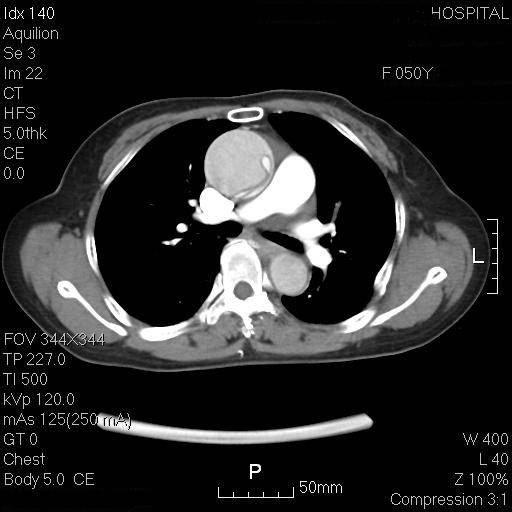
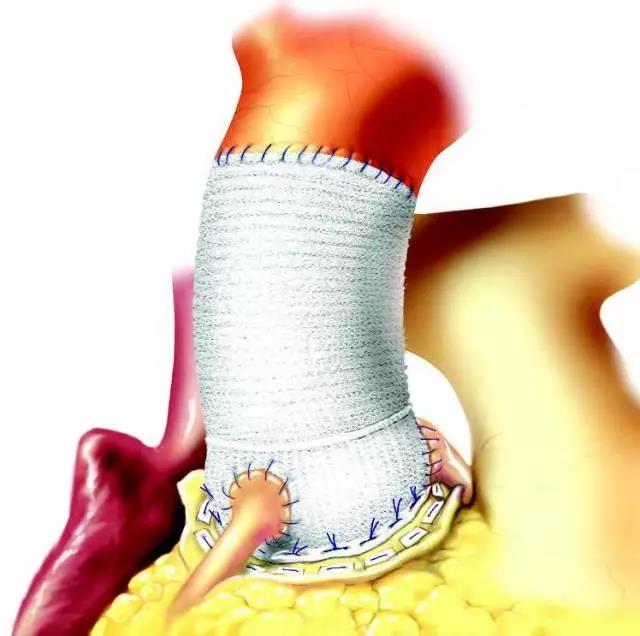
#动脉夹层#
27
#主动脉#
39
谢谢分享.学习了
56
学习一下知识了
48
学习了新知识
24
.学习了分享了
26
一起学习学习
27