Geroscience:SARS-CoV-2的持续病毒RNA脱落与住院COVID-19患者的谵妄发生率和6个月死亡率相关
2022-05-23 从医路漫漫 MedSci原创
持续的病毒脱落现象已得到充分研究,并在许多其他具有广泛公共卫生影响的病毒中得到证明,包括甲型禽流感和埃博拉。
背景:世界卫生组织宣布,新型冠状病毒病毒是导致2020年3月开始的2019年(新冠肺炎)全球疫情冠状病毒疾病的病毒。截至2022年2月,新冠肺炎已影响全球超过4.29亿人,并造成超过590万人死亡。大多数感染新型冠状病毒病毒的患者会有轻微的临床症状,但有些人会发展成严重的疾病,需要住院治疗和有创机械通气。这些患者面临着最高的死亡风险。核酸扩增检测,特别是实时逆转录聚合酶链反应(RT-PCR)检测,构成了诊断住院患者新型冠状病毒感染的临床标准。然而,RT-PCR检测持续或间歇阳性的患者给专家带来了临床难题。
对持续性病毒RNA脱落的评估是追踪严重病毒感染的恢复和长期反应的一种方法。持续病毒脱落的检测受初始疾病严重程度、病毒载量和样本来源的影响。持续的病毒脱落现象已得到充分研究,并在许多其他具有广泛公共卫生影响的病毒中得到证明,包括甲型禽流感和埃博拉。目前尚不清楚在住院患者的常规鼻咽拭子中持续检测到新型冠状病毒RNA是否代表复制病毒或仅仅是细胞碎片中的病毒核酸。此外,持续的RNA检测是否提供了关于住院患者的临床病程或发展为长期病毒后综合征的可能性的任何预后或机制信息,这一点尚未解决。因此,就持续阳性的新型冠状病毒RT-PCR检测的解释和风险向个人提供适当的建议变得具有挑战性。此外,对其他病毒的大量研究表明,持续病毒脱落的患者表现出功能失调的T细胞反应,患有严重疾病的住院患者具有更活跃和持续的病毒复制。在这种情况下,减弱的宿主免疫反应可能会减缓病毒清除,并导致持续的病毒脱落。严重的新冠肺炎病、男性和治疗延迟都是公认的病毒持续释放的危险因素。
目的:为了进一步了解住院新冠肺炎患者正在进行的临床护理并探索疾病机制,我们试图确定持续性病毒RNA脱落的患病率和风险因素,并评估其与谵妄(急性新冠肺炎的主要神经系统并发症)和住院新冠肺炎患者6个月死亡率的关系。
方法:我们回顾性评估了2020年3月至8月间西北医药保健(NMHC)患者的持续性病毒脱落情况。
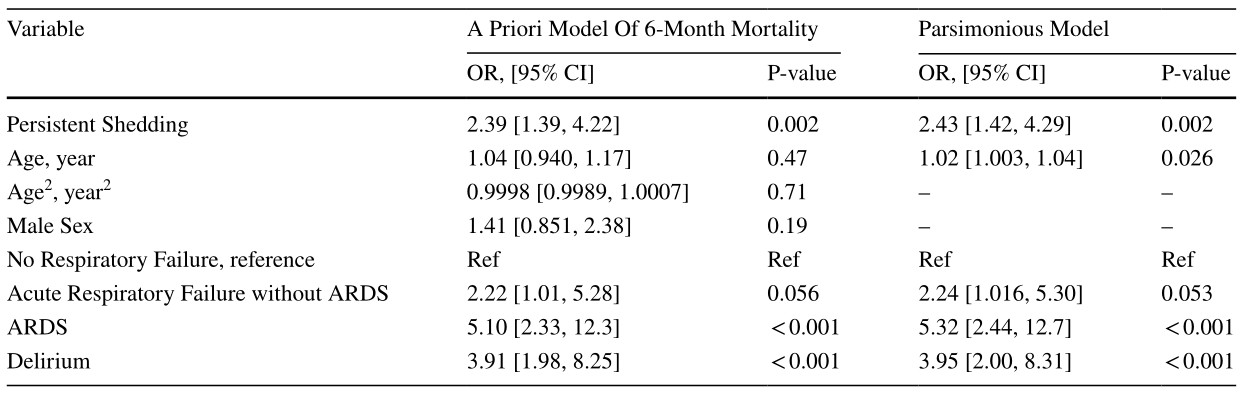
结果:在2518名经逆转录聚合酶链反应(RT-PCR)确诊为新冠肺炎的住院患者中,有959名患者在首次阳性检测后至少14天内重复进行了新型冠状病毒逆转录聚合酶链反应(RT-PCR)。其中,405名(42.2%)患者被发现有持续性病毒脱落。持续的病毒脱落与男性、身体质量指数增加、糖尿病、慢性肾脏疾病以及初次新冠肺炎住院期间暴露于皮质类固醇相关。在校正了包括呼吸功能障碍严重程度(OR 2.4595%可信区间为1.75,3.45)。即使在调整了年龄、呼吸功能障碍的严重程度和院内谵妄的发生率后,持续的病毒脱落仍然与6个月死亡率的增加显著相关(OR 2.4395%可信区间为1.42,4.29)。
表1 长期(证实> 14天)病毒RNA脱落模型
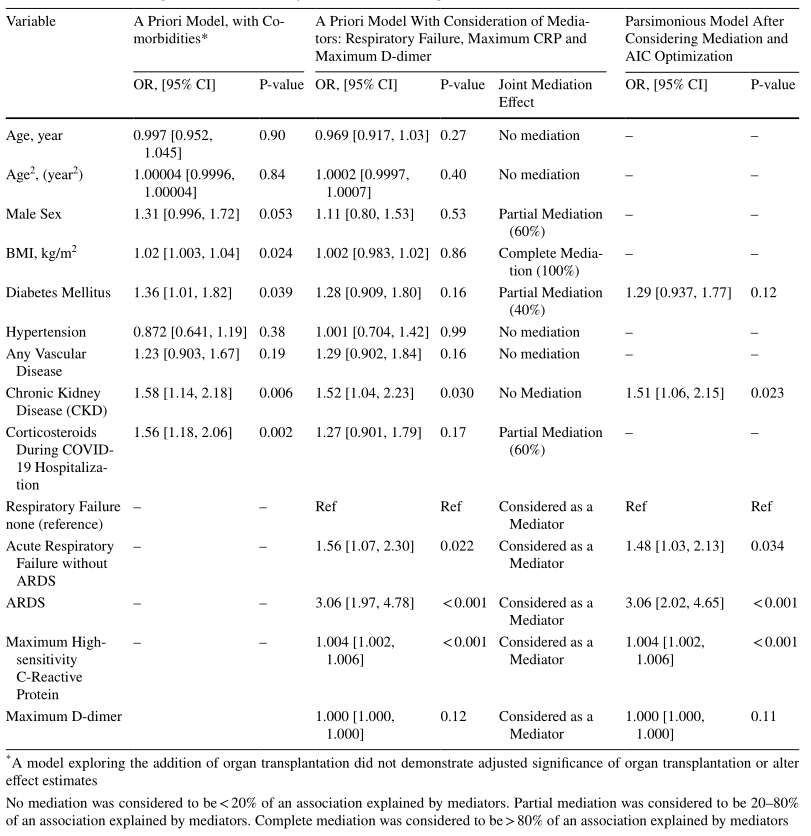
表2谵妄(曾经混淆评估方法阳性)和急性脑功能障碍的模型
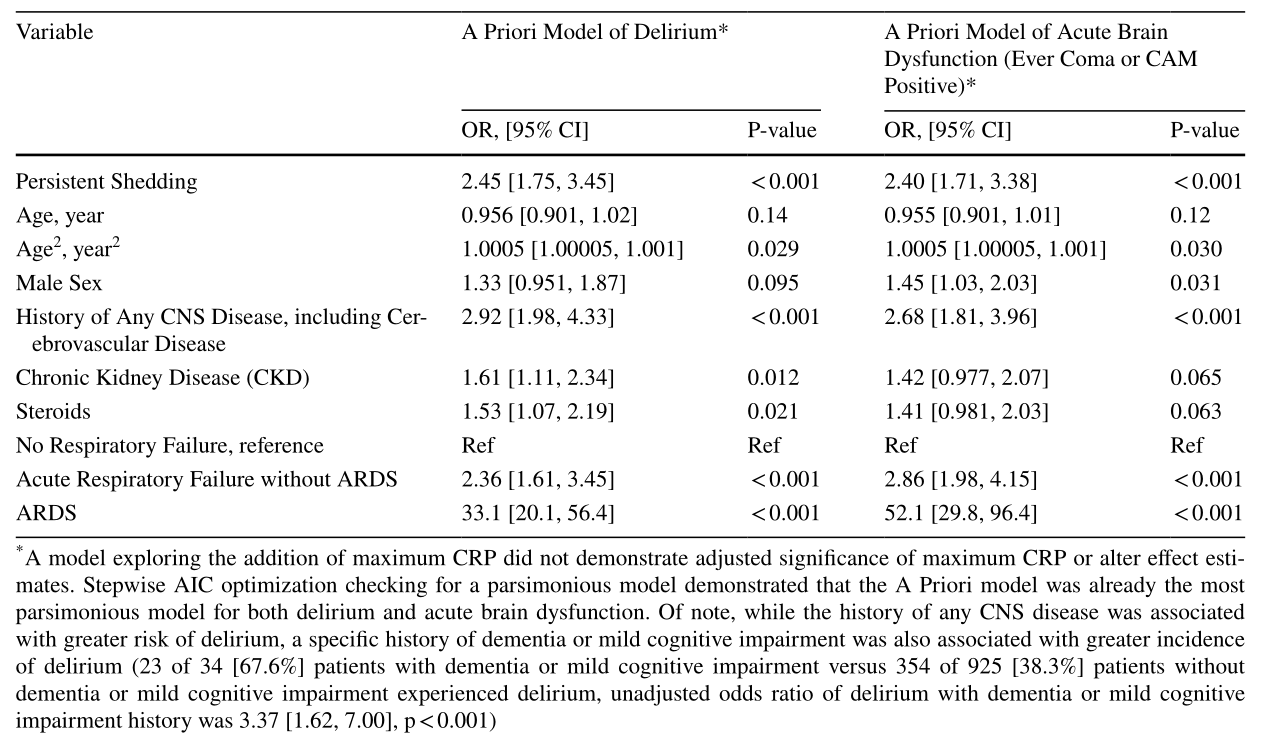
表3六个月死亡率模型
结论:持续性病毒脱落经常发生在住院的新冠肺炎患者中,并与院内谵妄和6个月死亡率增加相关。
原文出处:Batra A, Clark JR, Kang AK, et al.Persistent viral RNA shedding of SARS-CoV-2 is associated with delirium incidence and six-month mortality in hospitalized COVID-19 patients.Geroscience 2022 May 11
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#发生率#
126
#SARS-CoV#
116
#GER#
120
#COVID-19患者#
94
#SARS#
114
#ROS#
112
#SCIE#
72