预防系统性硬化病患者进一步发生肺动脉高压要靠。。。
2018-01-04 熊长明 肺血管病
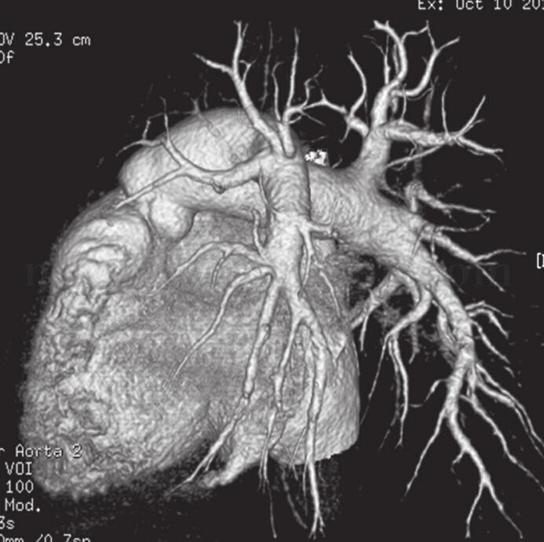
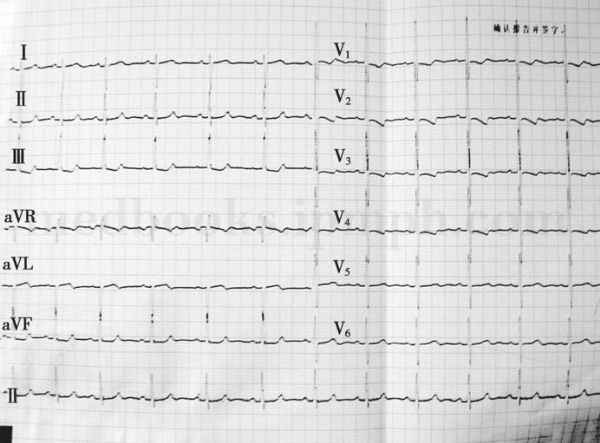
患者,女,50岁。因“活动后气短、乏力、心悸”来院就诊。外院超声心动图检查发现肺动脉高压和右心房、室扩大。患者既往有雷诺现象10年,2年前曾确诊系统性硬化症。患者此次来院诊断肺动脉高压是否与多年的系统性硬化症有关?还有其它疾病吗?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#系统性#
70
#动脉高压#
77
#系统性硬化#
66
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
76
学习学习学习
91
学习学习学习
102
学习学习学习
109
学习学习学习
82
学习学习学习
106
学习学习学习
68