Nature子刊:“换血大法”治疗阿尔茨海默病具有可行性!
2022-08-20 露娜 生物探索
AD是老年人群中最常见的痴呆症原因。数十年来,研究人员一直致力于了解AD的遗传和分子基础,但尚未发现有效的治愈或改善措施。
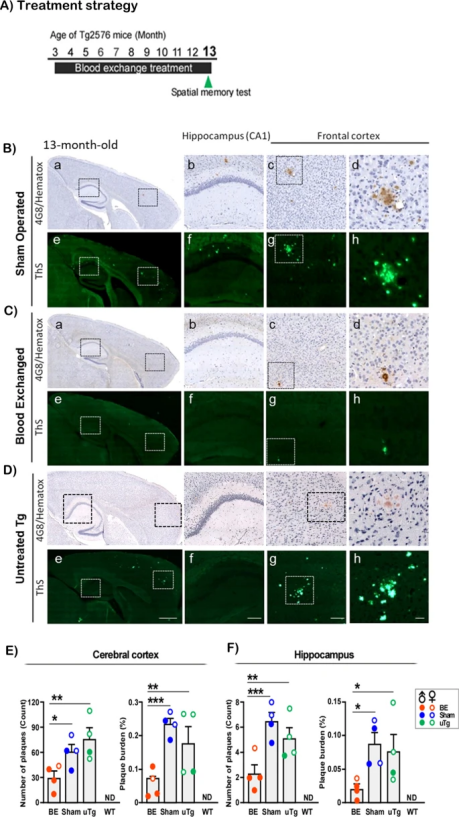
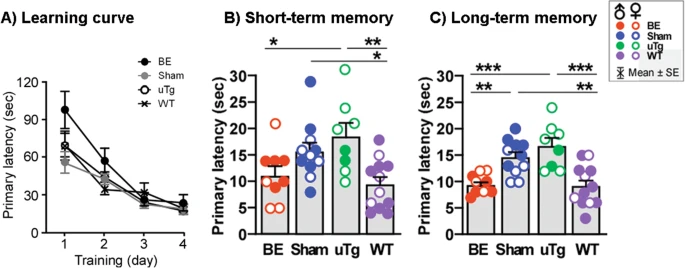
既往研究表明,β-淀粉样蛋白的错误折叠、聚集和脑沉积是诱发AD的主要因素,因此,预防和去除错误折叠的蛋白质聚集体是治疗AD的潜在策略,目前开展的治疗方法也多聚焦在预防或清除β-淀粉样蛋白。 近日,发表在Nature子刊Molecular Psychiatry上一篇题为“Preventive and therapeutic reduction of amyloid deposition and behavioral impairments in a model of Alzheimer’s disease by whole blood exchange”的研究表明,通过与健康小鼠进行全血交换,患有AD小鼠的大脑淀粉样斑块的形成显著减少了40-80%,这预示着换血治疗或可有效治疗阿尔茨海默病。 图1 研究成果(图源:[1]) 在假定外周循环会影响脑病理异常的前提下,研究人员尝试研究换血疗法对减少阿尔茨海默病病理的作用。研究者选用具有129S遗传背景的Tg2576小鼠作为AD的淀粉样变病理模型,由于这些小鼠携带淀粉样前体蛋白瑞典型突变基因,所以在成长到8-9个月大时,大脑中会表现出淀粉样沉积物。在Tg2576小鼠三个月大时,研究者从具有相同遗传背景的健康野生型小鼠中抽出“全血”,少量多次,来部分替换Tg2576小鼠的血液,连续进行10至14个月。 注:“全血”并非小鼠的全部血液,而是指未除去任何成分的血液 在该过程中,研究团队主要通过30号针头的肝素涂层注射器从颈静脉手动抽取300μL总血,然后将其缓慢注入(100 μL/min)到Tg2576小鼠的颈静脉中以补偿抽出的体积。重复6到8次这种换血操作,可实现每只动物每月1.8到2.4毫升的血液交换,这对应于每次手术时可替换原始血液的40%到60%。研究发现: 1. 换血疗法可显著减少老年鼠脑内淀粉样斑块的累积 实验中,在给携带阿尔茨海默病基因的小鼠多次进行输血治疗后发现,小鼠大脑中形成的淀粉样蛋白斑块减少了40%-80%;通过观察小鼠大脑矢状位横截面图,研究人员发现,在换血后的老年Tg2576小鼠脑内,仅观察到非常少量以及很小的脑淀粉样斑块;而相比之下,对照组老年小鼠的大脑皮层和海马体中,则出现了大量的脑淀粉样斑块(图2)。 图2 血液交换治疗可减少脑淀粉样斑块的积累(图源:[1]) 具体来说,接受全血疗法的老年小鼠脑内,淀粉样斑块的数量和覆盖面积都明显减少:与对照组相比,换血小鼠的大脑皮层和海马体中,淀粉样斑块的数量分别减少了50.0%和64.2%,覆盖面积分别减少了75.6%和75.9%。由此,不论从数量还是面积,换血疗法可有效地减少脑内斑块的形成。 2. 换血疗法可改善老年小鼠的空间记忆 为了研究血液交换是否会导致空间记忆的功能变化,在小鼠12.5个月大的时候对其进行时长1小时的巴恩斯迷宫测试,了解接受多次血液交换治疗的Tg2576小鼠的学习曲线(A)、短期记忆(B)和长期记忆(C)。研究团队分别在第5天、连续4天训练后评估短期记忆,在第12天评估长期记忆。 图3 血液交换治疗改善空间记忆(图源:[1]) 结果显示,具有病理性淀粉样斑块的老年小鼠,在经历输血治疗后,其空间记忆能力得到显著改善。 参考资料:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#阿尔茨海#
114
#阿尔茨#
104
#可行性#
138
#Nat#
65
全血交换
76
#阿尔茨海默#
108