Int J Urol:非转移性pT3a肾细胞癌的术后复发预测因素调查
2021-09-05 AlexYang MedSci原创
根治性肾切除和部分肾切除是非转移性RCC的根治性疗法。根治性手术患者的复发率约为30%,对于高风险复发患者需要进行密切随访。
根治性肾切除和部分肾切除是非转移性RCC的根治性疗法。根治性手术患者的复发率约为30%,对于高风险复发患者需要进行密切随访。

近期,来自日本的研究人员在《Int J Urol》发表文章,分析了肾外肿瘤扩展模式与其他病理因素,对非转移性pT3a肾细胞癌患者术后复发的影响。

研究人员调查了2006年至2017年间,在日本大阪关西医科大学医院接受根治性手术的587名非转移性肾细胞癌患者。从中筛选了114名主要组织学类型为pT3a的患者亚群,其中包括93名透明细胞肾细胞癌患者(81.6%),13名未分类的肾细胞癌患者(11.4%),6名嗜铬细胞肾细胞癌患者(5.3%)和2名乳头状肾细胞癌患者。主要终点是无复发生存期。采用了Kaplan-Meier方法和Cox比例风险模型进行统计分析。
在114名pT3a肾细胞癌患者中,42名患者(36.8%)出现复发。多变量分析显示,肾周脂肪浸润(风险比2.36,P=0.009),肉瘤或横纹肌瘤(风险比2.88,P=0.022)以及坏死(风险比2.34,P=0.030)是无复发生存的独立预测因素。那些有两个以上独立预测因素的高风险pT3a患者预后不佳。高风险pT3a患者与pT3b或以上患者的无复发生存期相似(中位无复发生存期分别为23.0和10.8个月)。
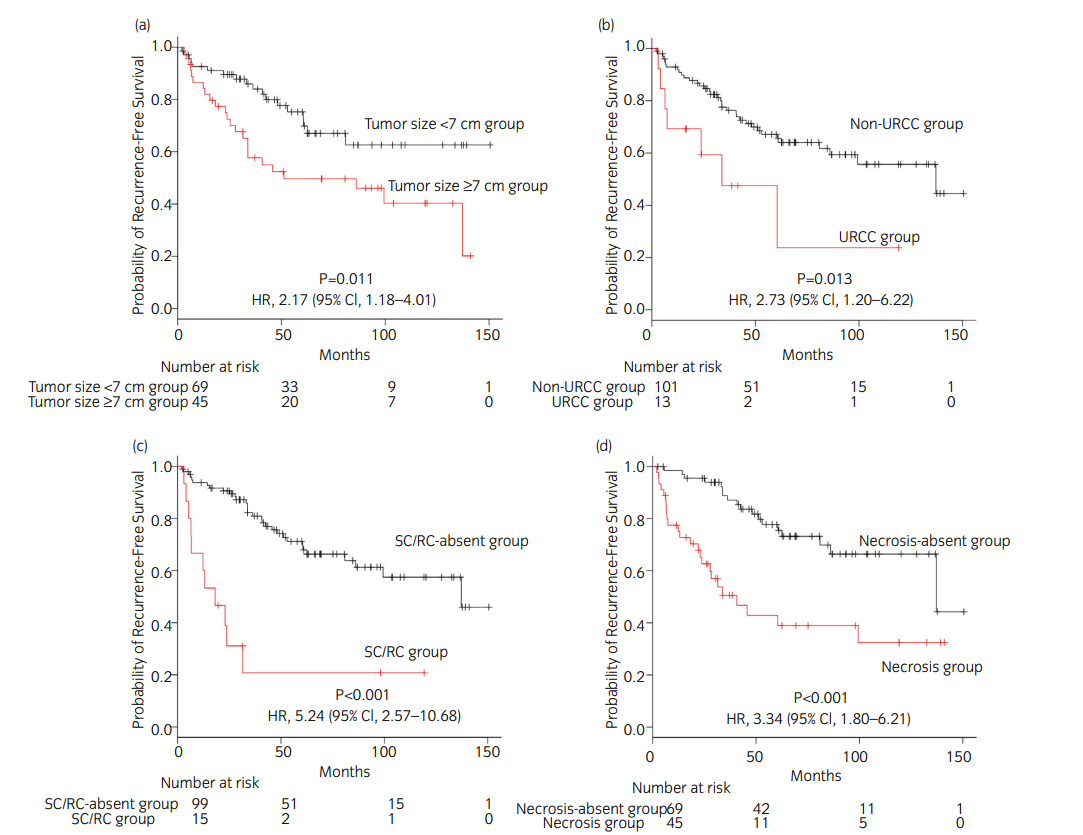
pT3a患者的RFS分层
综上所述,pT3a肾细胞癌患者中,肾周脂肪浸润、肉瘤或横纹肌以及坏死,是预测无复发生存的独立因素。有两个以上这些预测因素的患者预后较差。这些发现将有助于预测复发的风险分层,并为患者提供预后信息。
原始出处:
Haruyuki Ohsugi , Chisato Ohe , Takashi Yoshida et al. Predictors of postoperative recurrence in patients with non-metastatic pT3a renal cell carcinoma. Int J Urol. Aug 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#术后复发#
119
#非转移#
95
#细胞癌#
74
#非转移性#
103
#预测因素#
80
#转移性#
74
关注了
114