盘点:近期过敏性鼻炎研究进展盘点
2017-12-31 MedSci MedSci原创
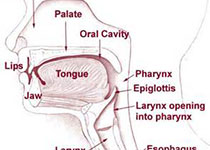
过敏性鼻炎主要由IgE介导的介质(主要是组胺)释放,并有多种免疫活性细胞和细胞因子等参与的鼻黏膜非感染性炎性疾病。其发生的必要条件有特异性抗原即引起机体免疫反应的物质、特应性个体、特异性抗原与特应型个体二者相遇。过敏性鼻炎是一个全球性健康问题,可导致许多疾病和劳动力丧失。梅斯医学小编整理了近期过敏性鼻炎的研究进展,与大家一起分享学习!【1】Clin Immunol:过敏性鼻炎患者对屋尘螨增
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#过敏性#
0
学习了.谢谢分享.
56
过敏性鼻炎新研究.学习了
58
#研究进展#
39
嗯嗯学习了
56
学习了谢谢分享
58
学习了受益匪浅
55
.阅
32