Thorax:COVID-19患者动静脉血栓栓塞患病率分析
2021-03-27 MedSci原创 MedSci原创
因严重COVID-19入住ICU的患者发生VTE的风险较高。
COVID-19患者静脉血栓栓塞事件(VTE)和动脉血栓栓塞事件(ATE)的发生率仍是未知的。

近日,胸部疾病领域权威杂志Thorax上发表了一篇研究文章,研究人员系统地检索了评估COVID-2019患者VTE和ATE患病率的观察性研究,检索时间截至2020年9月30日。
研究人员分析了102项研究(64503位患者)的结果。与COVID-19相关的VTE发生率为14.7%(95%CI为12.1%至17.6%,I2=94%;56项研究;16507名患者)。肺栓塞(PE)和腿部深静脉血栓形成的总体患病率分别为7.8%(95%CI为6.2%至9.4%,I2=94%;66项研究;23117名患者)和11.2%(95%CI为8.4%至14.3%,I2=95%;48项研究;13824名患者)。很少有孤立性亚节段性PE。
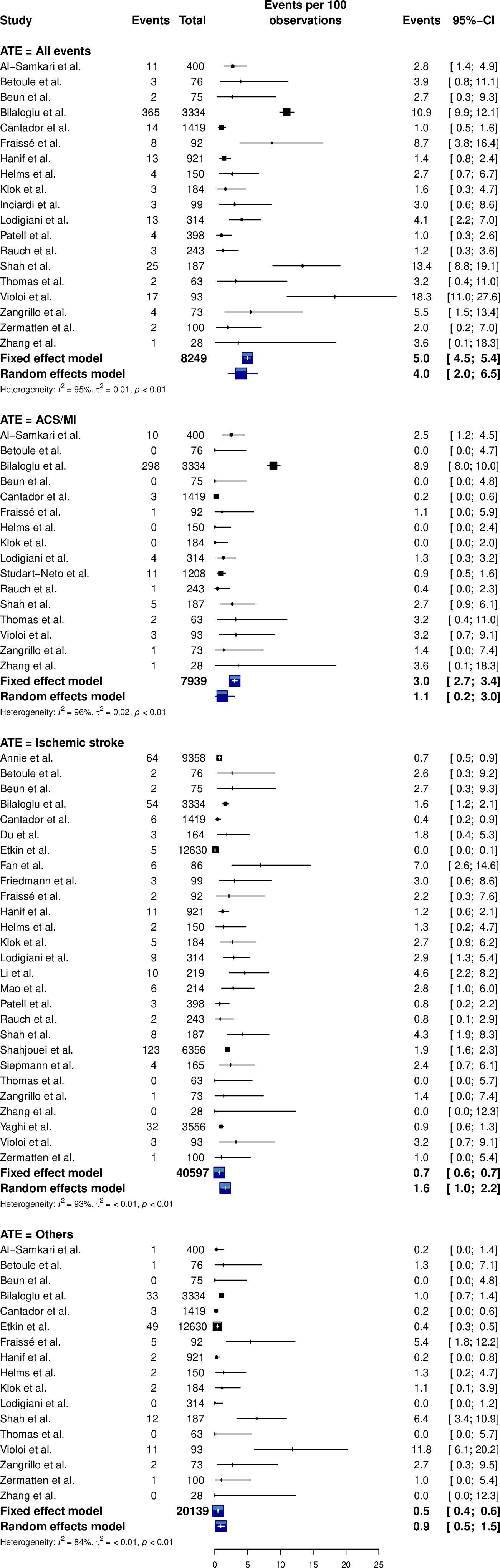
重症监护病房(ICU)患者的VTE患病率更高(23.2%,95%CI为17.5%至29.6%,I2=92%,vs. 9.0%,95%CI为6.9%至11.4%,I2=95%;P<0.0001)。总体ATE、急性冠脉综合征、卒中和其他ATE的发生率分别为3.9%(95%CI为2.0%至3.0%,I2=96%; 16项研究;7939例患者)、1.6%(95%CI为1.0%至2.2%,I2=93%;27项研究;40597名患者)和0.9%(95%CI为0.5%至1.5%,I2=84%;17项研究;20139名患者)。Meta回归和亚组分析未能解释整个ATE的异质性。高度异质性限制了评估的价值。
由此可见,因严重COVID-19入住ICU的患者发生VTE的风险较高。
原始出处:
Boun Kim Tan,et al.Arterial and venous thromboembolism in COVID-19: a study-level meta-analysis.Thorax.2021.https://thorax.bmj.com/content/early/2021/03/24/thoraxjnl-2020-215383
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉#
61
#静脉血#
70
#患病率#
73
#COVID-19患者#
79
我学到了很多东西谢谢老师
113